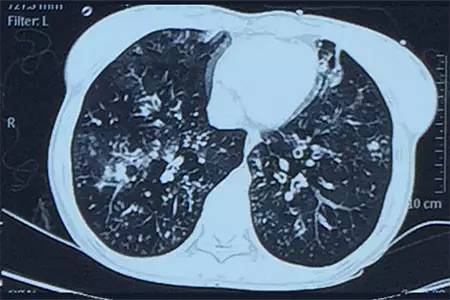
J Aller Cl Imm-Pract:支气管扩张患者中慢性鼻窦炎的患病率和临床意义
2019-03-08 xing.T 网络
由此可见,62%的支气管扩张成人患有CRS。它的存在与较差的HRQOL、更严重的疾病严重程度和更广泛的影像学支气管扩张相关。
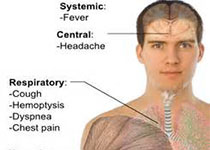
慢性鼻窦炎(CRS)是一些支气管扩张患者的肺外表现,但该人群中CRS的患病率及其临床影响尚未得到系统评价。近日,过敏性疾病领域权威杂志Journal of Allergy and Clinical Immunology-In Practice上发表了一篇研究文章,该系统评价旨在确定支气管扩张患者CRS的患病率并确定其临床意义。
研究人员检索了四个数据库,检索时间从数据库成立开始到2018年8月,确定了报告CRS在支气管扩张患者中的患病率和/或临床影响的研究。临床结局包括与健康相关的生活质量(HRQOL)、支气管扩张的严重程度、肺功能、临床和心理症状、恶化频率和医疗保健利用率。由两名独立评审员使用普遍性试验工具的偏倚风险对证据质量进行评级。
在确定的80项研究中,研究人员纳入了8项研究,包含797名参与者(所有成年人)。预测的平均FEV1%为77.7%。总体而言,五项研究被归类为低偏倚风险,三项具有中度偏倚风险。临床和/或影像学CRS的合并患病率为62%(95%CI为50%至74%)。CRS与更大程度的支气管扩张严重程度、较差的HRQOL、嗅觉灵敏度减少、炎症标志物水平升高和首次恶化时间缩短有关。然而,与气流阻塞的关联不一致,并且对焦虑或抑郁没有影响。
由此可见,62%的支气管扩张成人患有CRS。它的存在与较差的HRQOL、更严重的疾病严重程度和更广泛的影像学支气管扩张相关。
原始出处:
Emma Handley,et al.Prevalence and clinical implications of chronic rhinosinusitis in people with bronchiectasis: a systematic review. J Aller Cl Imm-Pract. 2019. https://www.jaci-inpractice.org/article/S2213-2198(19)30203-X/abstract
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支气管#
31
#扩张#
32
#患病率#
34
#ALL#
26
#慢性鼻窦炎#
34