SCI REP:二甲双胍和阿托伐他汀合用降低高胆固醇饮食的动脉粥样硬化作用!
2017-05-21 xing.T MedSci原创
总之,该研究结果表明阿托伐他汀/二甲双胍联合治疗可能会达到额外的抗动脉粥样硬化的益处,可能是通过增加巨噬细胞胆固醇流出。
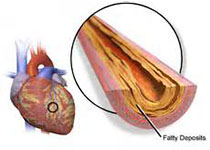
他汀类药物被广泛用于降低心血管风险。不幸的是,虽然服用了高剂量的他汀类药物,一些患者仍然经历了心血管事件。二甲双胍是一种抗糖尿病药物,据报道其具有抗动脉粥样硬化的作用。近日,Scientific reports 杂志上发表了一篇研究文章,研究人员旨在评估二甲双胍与阿托伐他汀联合使用是否能获得更多的益处。
在高胆固醇饮食喂养的兔子模型中,研究人员评估了联合治疗对动脉粥样硬化斑块、血脂、血糖水平、肝和肾功能的影响。同时在体外评估了联合用药对胆固醇外流及相关转运蛋白表达的影响。
研究人员的研究结果表明,联合治疗可以显著减少动脉粥样硬化病变面积,相比于阿托伐他汀没有额外的降脂效应。联合治疗显著增加高密度脂蛋白亚组的比例。静脉葡萄糖耐量试验表明接受阿托伐他汀治疗的兔在大剂量葡萄糖注射后随时间变化的血糖水平曲线下面积增加,而这可以被二甲双胍治疗完全逆转。在培养的巨噬细胞中,二甲双胍和阿托伐他汀联合治疗可以促进胆固醇流出和上调ATP结合盒转运体A1和G1的表达。
总之,该研究结果表明阿托伐他汀/二甲双胍联合治疗可能会达到额外的抗动脉粥样硬化的益处,可能是通过增加巨噬细胞胆固醇流出。
原始出处:
Fei Luo, et al. Combined use of metformin and atorvastatin attenuates atherosclerosis in rabbits fed a high-cholesterol diet. Scientific reports. 2017. https://www.nature.com/articles/s41598-017-02080-w
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#粥样硬化#
33
二甲双胍和阿托伐他汀的合用。
68
学习
49
老药新用途,需要临床细心观察
81
药物联合治疗的临床观察
63
文章真好,拜读了
53
学习了谢谢分享。
29
学习。。。。。。。。
31
学习了
30
很不错,学习了!谢谢分享!
34