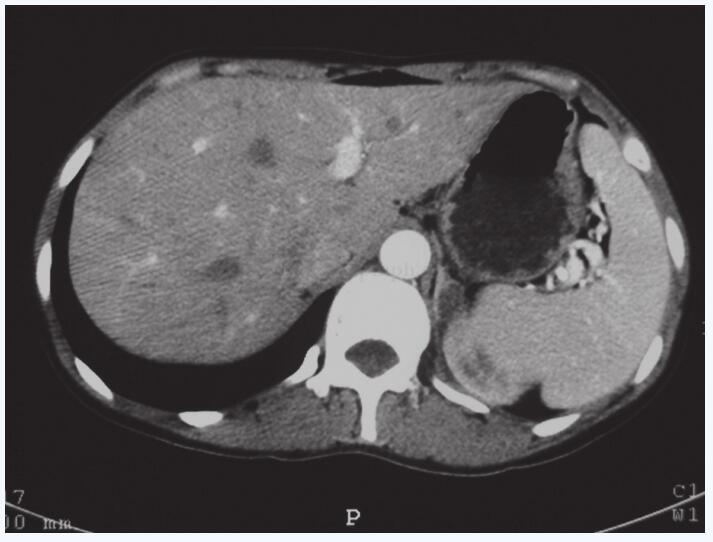
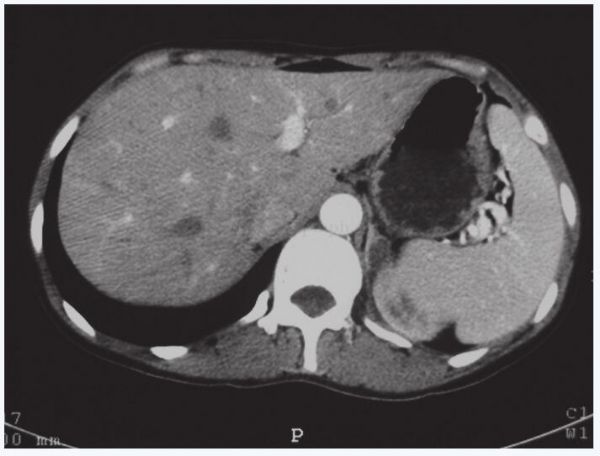
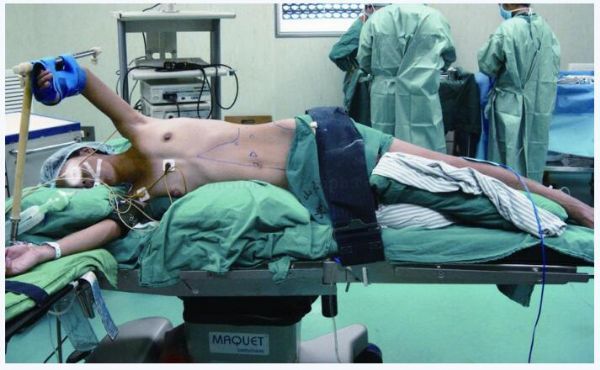
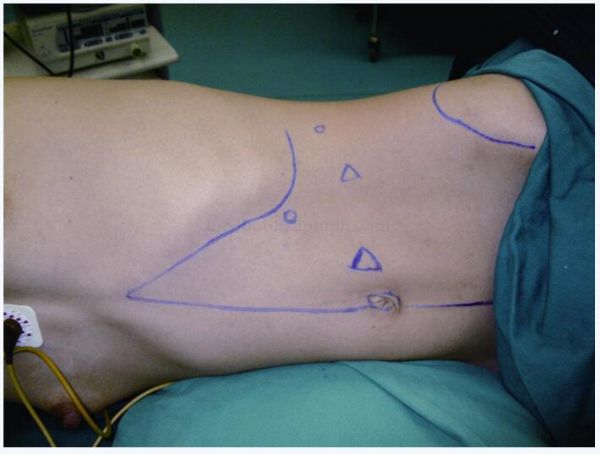
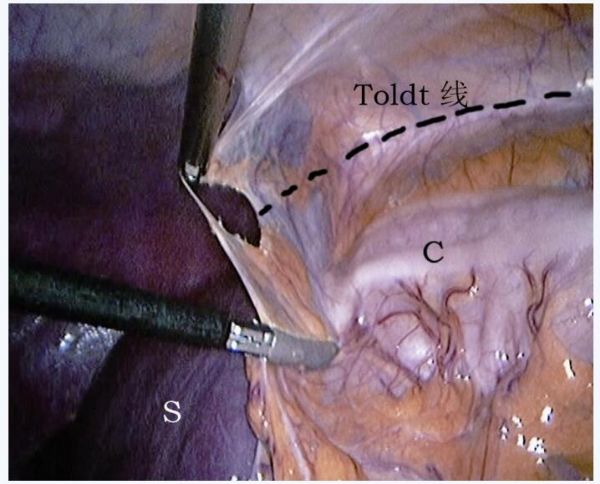
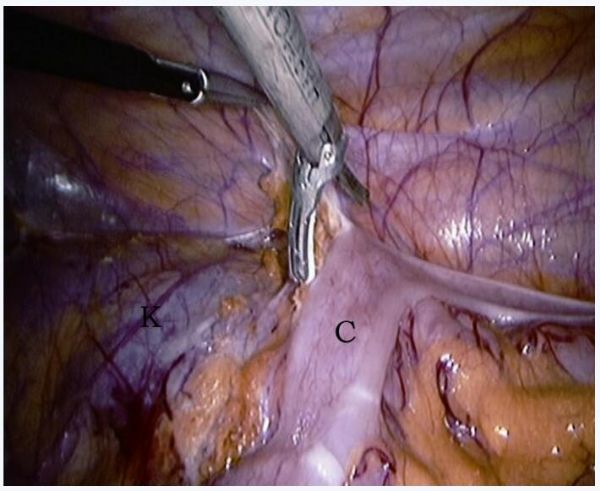
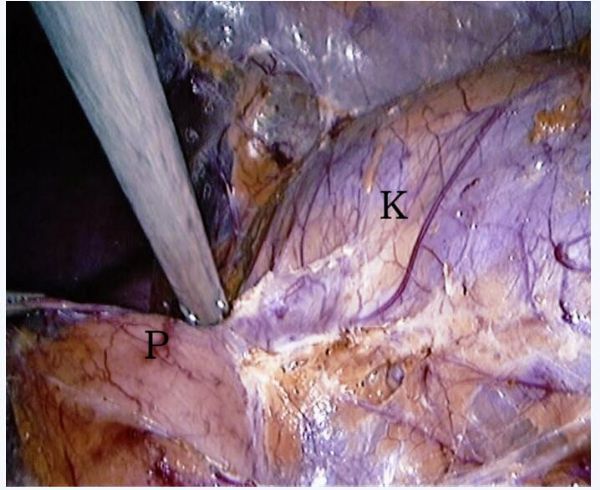
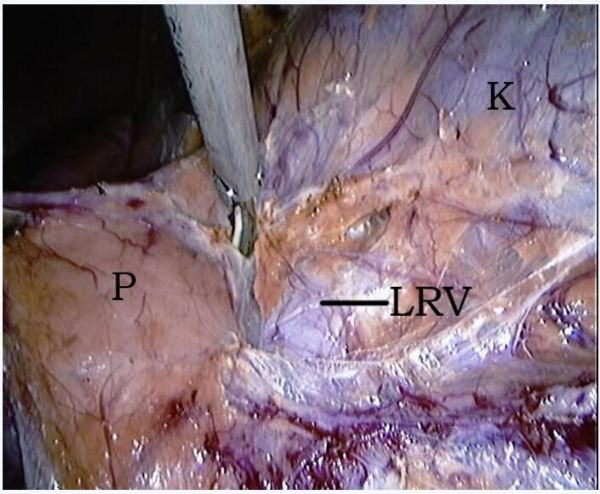
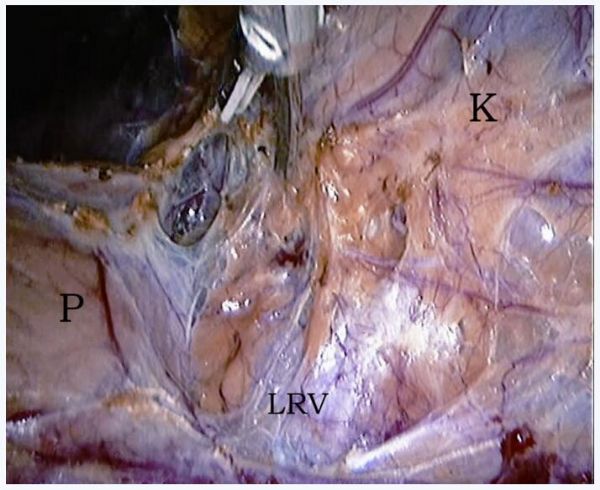
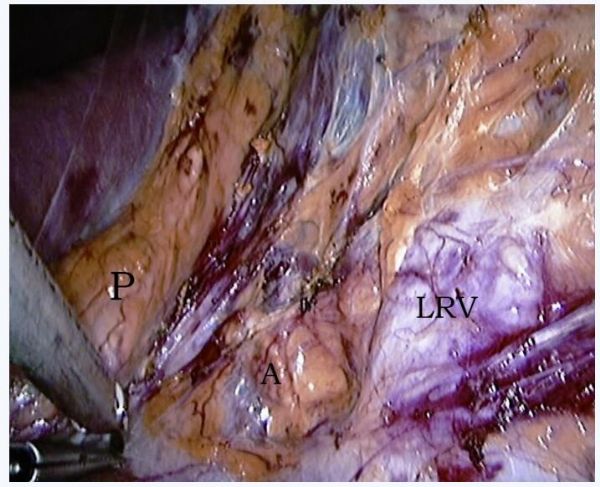
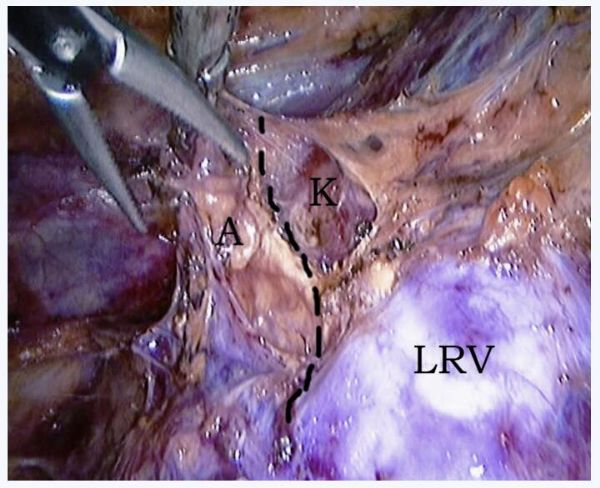
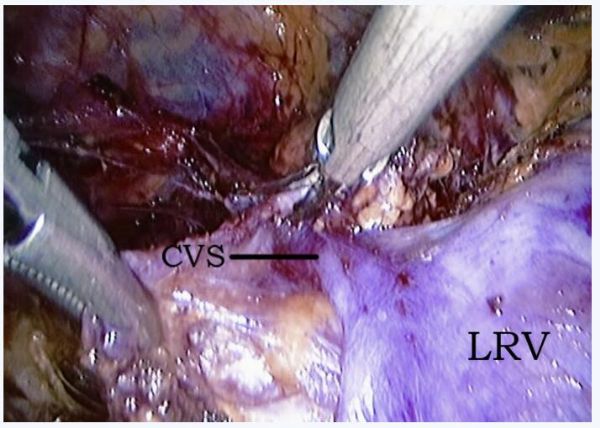
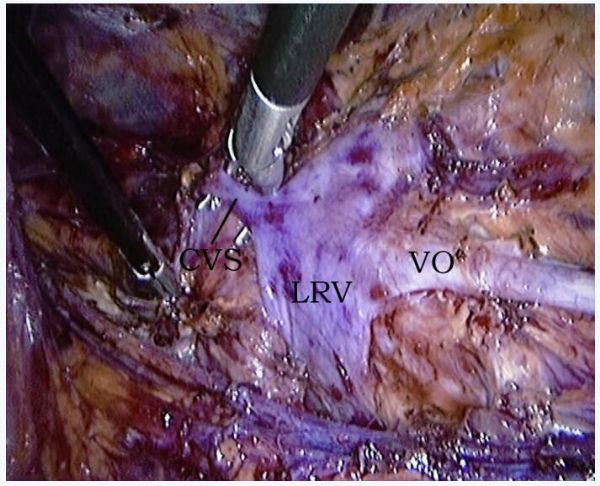
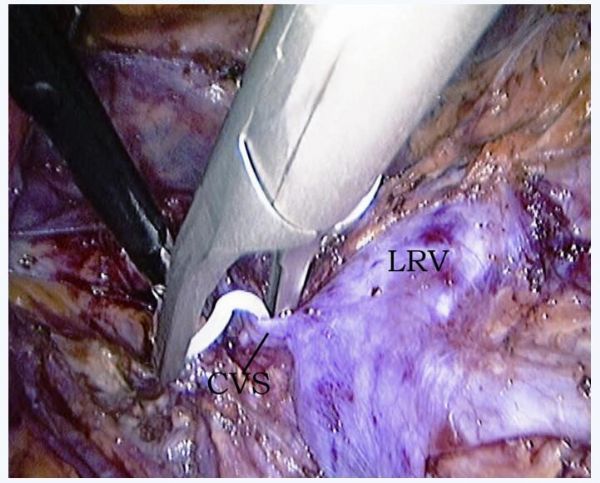
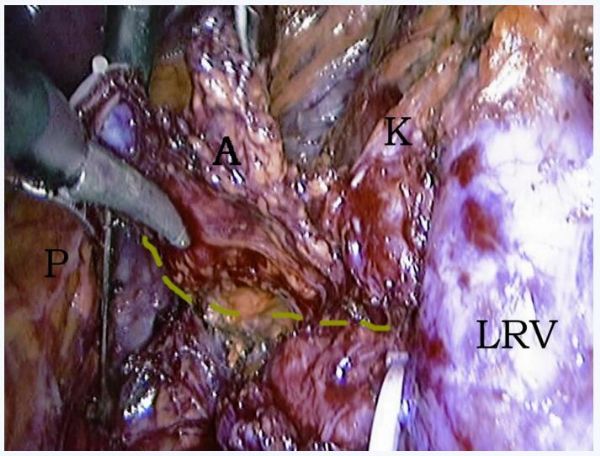
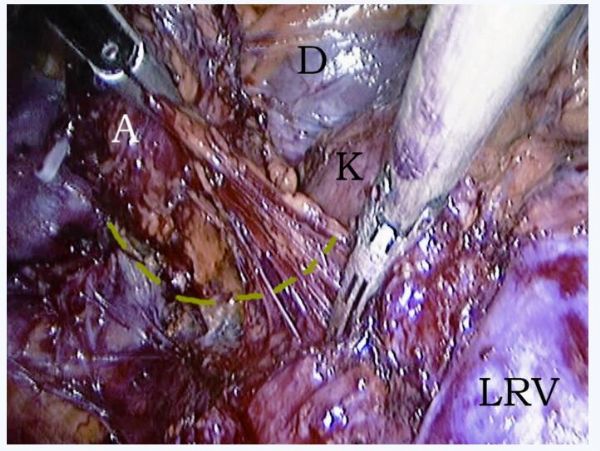
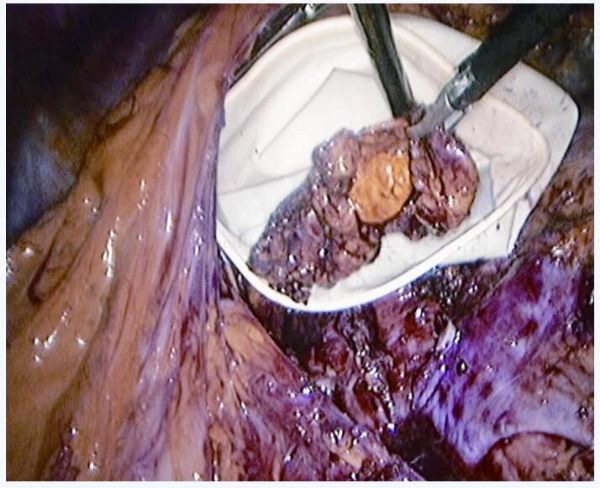
腹腔镜肾上腺肿瘤切除术手术图谱
2017-11-08 周芳坚 韩辉 泌尿生殖系肿瘤外科手术图谱
40岁女性确诊肾上腺原发性醛固酮增多症,术前准备和手术具体步骤,详见以下手术图谱——
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#肾上腺#
54
#肿瘤切除#
58
#切除术#
52
很好的图谱.已分享给同事
95
#腹腔镜#
45
#肾上腺肿瘤#
42
学习了受益匪浅
71