Ann Oncol: Ribociclib联合氟维司群治疗HR+/HER2-晚期乳腺癌的疗效和安全性:III期临床研究MONALEESA-3的结果更新
2021-06-27 yd2015 MedSci原创
MONALEESA-3研究证实,Ribociclib联合氟维司群较安慰剂联合氟维司群明显改善HR+/HER2-晚期乳腺癌患者的OS。
III期临床研究MONALEESA-3是在30个国家170个中心开展的随机、双盲、安慰剂对照研究,评估Ribociclib联合氟维司群对比安慰剂联合氟维司群治疗HR+/HER2-晚期乳腺癌的疗效和安全性。前期分析结果表明,Ribociclib联合氟维司群较安慰剂联合氟维司群明显改善患者的PFS(20.5 vs 12.8 个月,HR=0.59; 95%CI 0.48-0.73, P < 0.001)和OS(未达到vs 40.0个月,HR=0.72; 95% CI 0.57-0.92; P=0.00455)。Annals of Oncology杂志更新了长期随访结果。
从2015年6月18日到2016年6月10日,共纳入726例患者,其中484名患者被分配到Ribociclib组,242名患者被分配到安慰剂组。中位随访56.3个月,Ribociclib组和安慰剂组的中位OS分别为53.7个月(95% CI 46.9-NR)和41.5个月 (95% CI 37.4-49.0) (HR, 0.73; 95% CI 0.59-0.90)。4年生存率分别为54% (95% CI 49% to 58%) 和45% (95% CI 38% to 51%)。5年生存率分别为46% (95% CI 40% to 52%) 和31% (95% CI 23% to 40%)。
其中365例患者接受研究的治疗方案为一线治疗,两组的中位OS分别为未达到 (95% CI 59.9-NR)和51.8个月(95% CI 40.4-57.6) (HR=0.64; 95% CI 0.46-0.88)。4年OS率分别66% (95% CI 59% to 72%) 和53% (95% CI 44% to 62%);而5年OS率分别54% (95% CI 41% to 65%)和36% (95% CI 23% to 49%)。
347例患者接受研究的治疗方案为二线治疗,两组的中位OS为39.7个月(95% CI 37.4-46.9) 和33.7个月(95% CI 27.8-41.3) (HR=0.78; 95% CI 0.59-1.04)。4年OS率分别为39.7个月(95%CI 37.4-46.9) 和33.7个月(95% CI 27.8-41.3) (HR=0.78; 95% CI 0.59-1.04)。
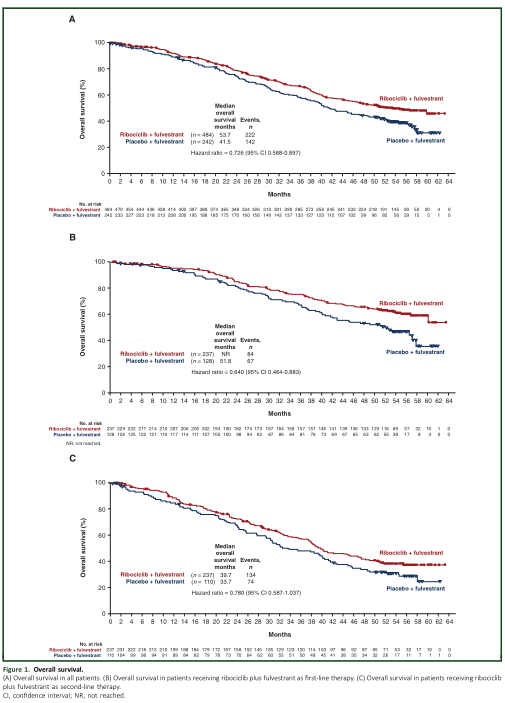
OS
364例患者伴有肺或肝脏转移,两组中位OS分别为46.9个月(95% CI 38.1-NR)和39.4个月(95% CI 29.9-44.9) (HR, 0.73;95% CI 0.55-0.98)。
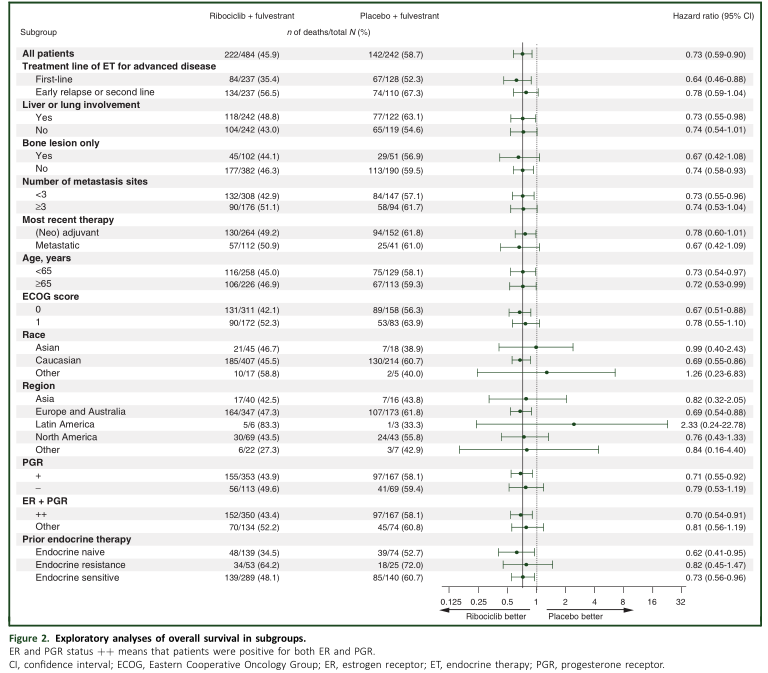
亚组OS分析
PFS2定义为随机化开始至第二次进展或死亡的时间。两组的中位PFS2分别为37.4个月(95% CI 31.1-42.6) 和 28.1个月 (95% CI 24.0-31.6) (HR=0.7069; 95% CI 0.57-0.84)。作为一线治疗时,两组的中位PFS2分别为53.7和35.5个月(HR, 0.63; 95% CI 0.47-0.84)。作为二线治疗时,中位PFS2分别为26.0和20.5个月(HR=0.73; 95% CI 0.56-0.96)。

PFS2
严重不良事件跟之前报道的一致。中性粒细胞减少(Ribociclib组为58.2%; 安慰剂组为0.8%)是最常见的3或4级不良事件。特别关注的3或4级不良事件有肝胆毒性(Ribociclib组为13.9%,安慰剂组为6.2%)和QT间期延长(Ribociclib组为3.1%,安慰剂组为1.2%)。
综上,MONALEESA-3研究证实,Ribociclib联合氟维司群较安慰剂联合氟维司群明显改善HR+/HER2-晚期乳腺癌患者的OS。
原始出处:
D J Slamon, P Neven, S Chia, et al. Ribociclib plus fulvestrant for postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer in the phase 3 randomized MONALEESA-3 trial: updated overall survival. Ann Oncol. 2021 May 15;S0923-7534(21)01553-2. doi: 10.1016/j.annonc.2021.05.353. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效和安全性#
33
#III期临床研究#
44
#I期临床#
35
#HER2-#
38
#Oncol#
31
#II期临床研究#
32
#III#
36
#ribociclib#
35
#II期临床#
42
#III期#
27