JAHA:心源性休克患者右心导管与结局改善相关
2021-08-22 MedSci原创 MedSci原创
心源性休克患者RHC的使用与患者结局改善和心力衰竭疗法使用增加有关。
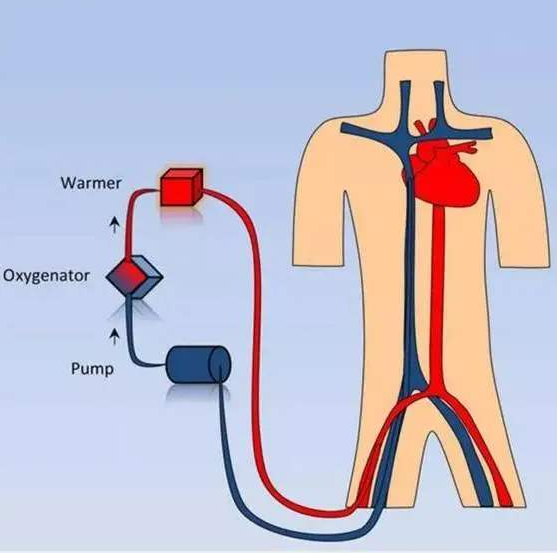
右心导管插入术(RHC)的用处长期以来一直存在争议,近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在探究使用RHC治疗心源性休克的真实世界数据。
在使用国际疾病分类第十次修订版(ICD-10)的全国再入院数据库中,研究人员确定了2016年至2017年期间因心源性休克住院的236156名患者。研究人员试图评估RHC在住院期间对治疗策略、并发症、结局以及30天再入院率的影响。
 该研究共有25840名患者(9.6%)在首次入院时接受了RHC。与非RHC组相比,RHC组的合并症显著更多。在首次入院期间,RHC组的死亡率(25.8% vs. 39.5%,P<0.001)和卒中发生率(3.1% vs. 3.4%,P<0.001)较低。
该研究共有25840名患者(9.6%)在首次入院时接受了RHC。与非RHC组相比,RHC组的合并症显著更多。在首次入院期间,RHC组的死亡率(25.8% vs. 39.5%,P<0.001)和卒中发生率(3.1% vs. 3.4%,P<0.001)较低。
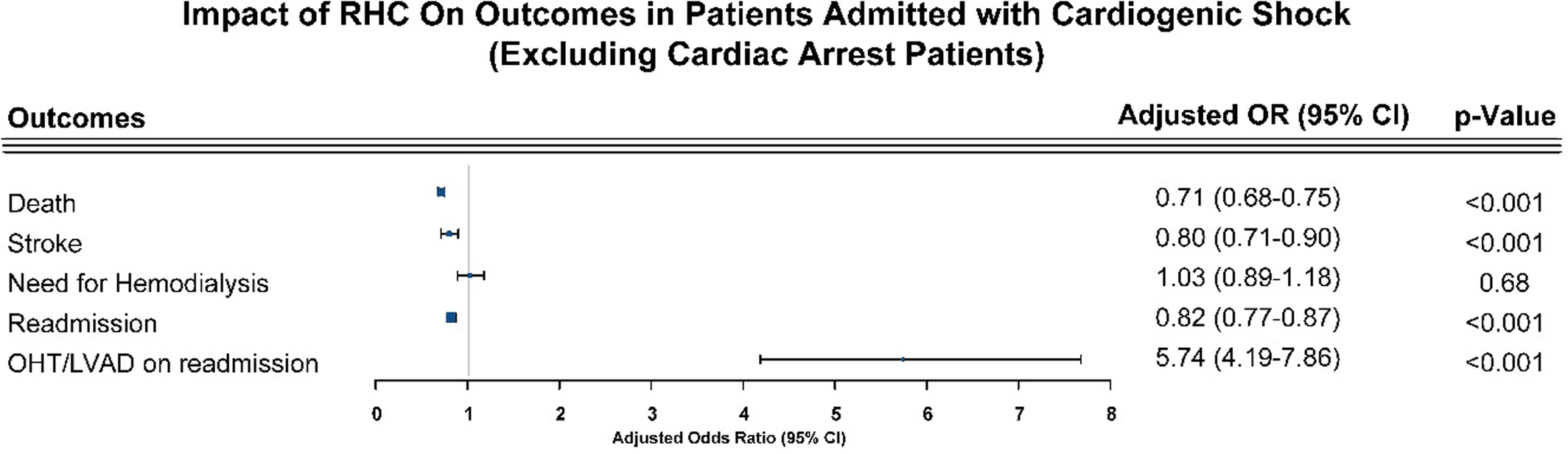 RHC组30天再入院率(18.7% vs. 19.7%,P=0.04)和再入院死亡率(7.9% vs. 9.3%,P=0.03)也较低。调整后,RHC与较低的指数入院死亡率(比值比为0.69;95%CI为0.66–0.72)、较低的卒中率(比值比为0.81;95%CI为0.72–0.90)、较低的30天再入院率相关(比值比为0.83;95%CI为0.78–0.88)和更高的左心室辅助装置植入/原位心脏移植率(比值比为6.05;95%CI为4.43–8.28)相关。排除心脏骤停患者后,结果没有显著差异。
RHC组30天再入院率(18.7% vs. 19.7%,P=0.04)和再入院死亡率(7.9% vs. 9.3%,P=0.03)也较低。调整后,RHC与较低的指数入院死亡率(比值比为0.69;95%CI为0.66–0.72)、较低的卒中率(比值比为0.81;95%CI为0.72–0.90)、较低的30天再入院率相关(比值比为0.83;95%CI为0.78–0.88)和更高的左心室辅助装置植入/原位心脏移植率(比值比为6.05;95%CI为4.43–8.28)相关。排除心脏骤停患者后,结果没有显著差异。
由此可见,心源性休克患者RHC的使用与患者结局改善和心力衰竭疗法使用增加有关。需要进一步的盲法随机研究来证实这些发现。
原始出处:
Sagar Ranka.et al.Right Heart Catheterization in Cardiogenic Shock Is Associated With Improved Outcomes: Insights From the Nationwide Readmissions Database.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019843
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#右心导管#
31
#AHA#
38
#心源性休克#
40
#心源性#
43