Diabetes care:1型糖尿病青年患者中血脂异常的预测因子
2017-01-29 MedSci MedSci原创
了解与1型糖尿病青年患者的血脂异常进展和消退相关的风险因素可能有助于指导疾病的治疗。近期,一项发表在Diabetes care杂志上文章进行了一项关于此的研究。此项研究在基线时研究了1,478名1型糖尿病青少年患者(年龄为10.8±3.9岁,50%为男性,77%为非西班牙裔白人,不使用降脂药);在青少年糖尿病(SEARCH)的平均随访时间为7.1±1.9年。进展为血脂异常的定义为在基线时脂质浓度正
了解与1型糖尿病青年患者的血脂异常进展和消退相关的风险因素可能有助于指导疾病的治疗。
近期,一项发表在Diabetes care杂志上文章进行了一项关于此的研究。
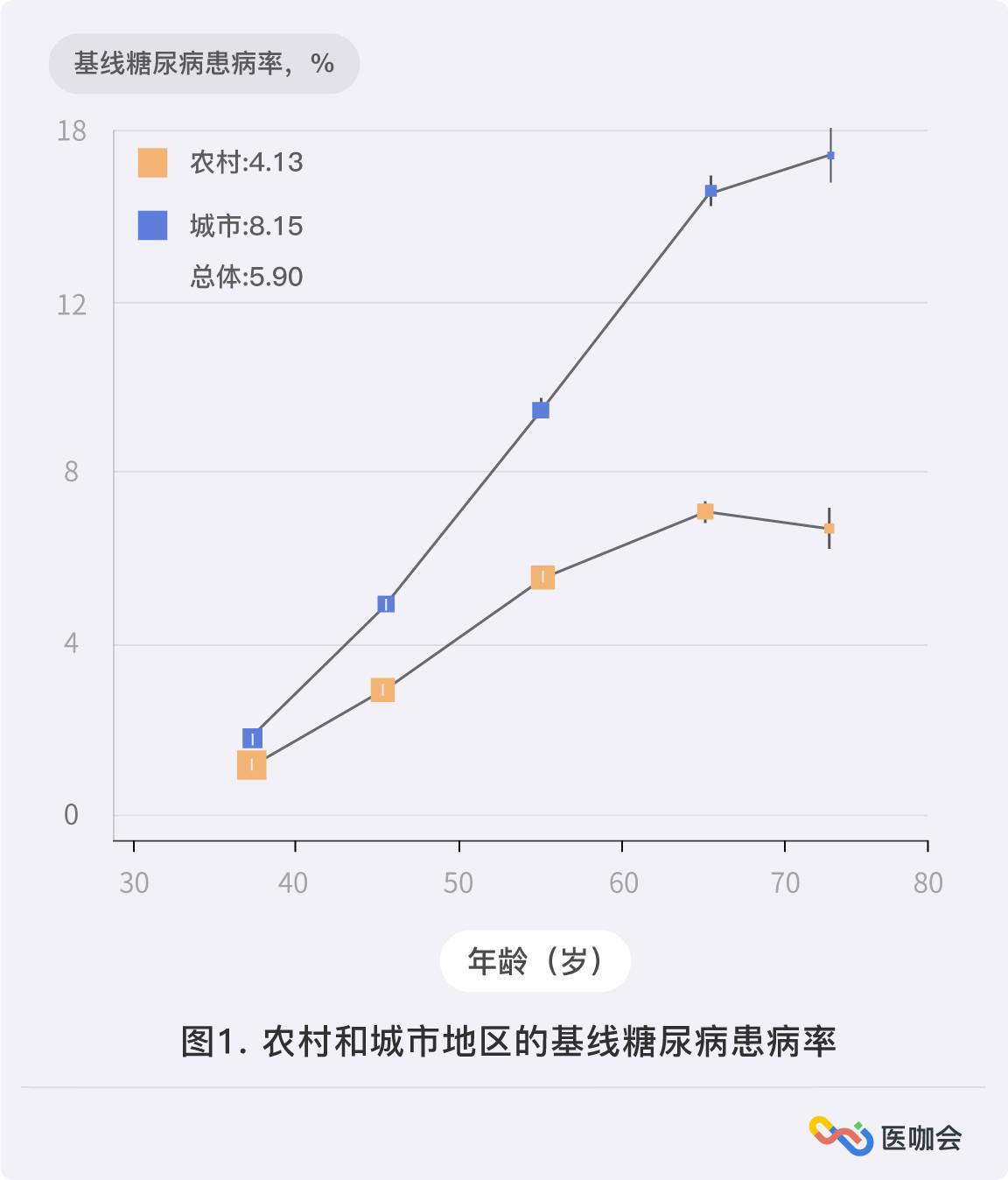
此项研究在基线时研究了1,478名1型糖尿病青少年患者(年龄为10.8±3.9岁,50%为男性,77%为非西班牙裔白人,不使用降脂药);在青少年糖尿病(SEARCH)的平均随访时间为7.1±1.9年。进展为血脂异常的定义为在基线时脂质浓度正常,而在随访时脂质浓度不正常(非HDL-胆固醇[C]>130mg/dL或HDL-C<35mg/dL)。回归定义为基线时脂质异常而随访时脂质正常。
研究结果显示:1型糖尿病青年中非HDL-C进展、回归、稳定正常、及稳定的异常分别为19%、5%、69%和7%。HDL-C的相应百分比分别为3%、3%、94%和1%。与非HDL-C进展相关的因素是男性患者更高的A1C AUC和更高的WHtR AUC。非HDL-C回归与较低的WHtR AUC相关,HDL-C进展与男性性别和较高的WHtR AUC相关。HDL-C回归由于数字小而未建模分析。
此项研究结果表明:A1C和WHtR是与1型糖尿病青年血脂异常随时间变化相关的可以改变的危险因素。
原始出处:
Shah AS, Maahs DM, Stafford JM, et al. Predictors of Dyslipidemia Over Time in Youth With Type 1 Diabetes: For the SEARCH for Diabetes in Youth Study. Diabetes Care. 2017 Jan 26. pii: dc162193. doi: 10.2337/dc16-2193.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Diabetes#
35
#BET#
33
#DIA#
30
好文,值得点赞,值得拥有,值得收藏!
68
#青年患者#
40
学习了,感谢
60
A1C和WHtR是与1型糖尿病青年血脂异常随时间变化相关的可以改变的危险因素。
72
继续学习
88
好文,值得学习
64
继续学习中
20