Ann Oncol :BRAF突变结直肠癌的诊治现状与展望
2017-08-01 佚名 肿瘤资讯
Josep Tabernero教授来自巴塞罗那瓦尔德西布伦大学医院,是肿瘤内科的主任,Tabernero教授将于2018-2019年担任ESMO的主席。Tabernero教授在结直肠的靶向治疗领域领导了一系列的I-II期临床试验,近期,在ESMO官方杂志Annals of Oncology发表了一篇综述,全面介绍了BRAF突变的结直肠癌,现将主要内容进行了提炼。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
25
#诊治现状#
0
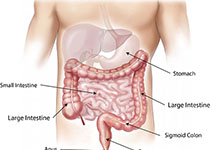
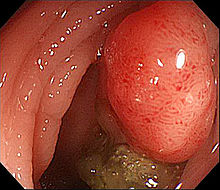
BRAF突变结直肠癌.
0
学习了,谢谢作:者分享!
55
学习了,谢谢作者分享!
55
学习了,谢谢作者分享!
68
学习了,谢谢作者分享!
45
学习一下知识
26
#BRAF#
24
#结直肠#
0