干货:晕厥的诊断与治疗
2016-10-05 Joy 医学界神经病学频道
晕厥是指短暂的意识丧失和不能维持直立姿势,特点是起病迅速、持续时间短,并能自然、快速而完全恢复。晕厥可使人失健、致人受伤、诊治费钱,更重要的是它可能是猝死的前奏。一组数据显示,年龄在 15~35 岁之间的 162 位猝死病人中,25% 开始时表现为晕厥。因此,我们必须对各种晕厥和类似晕厥做出鉴别诊断,再对其致猝死的危险性做出判断。以采取合适的防治措施,防止其复发、减少其损伤、避免发生猝死。晕厥的常
晕厥是指短暂的意识丧失和不能维持直立姿势,特点是起病迅速、持续时间短,并能自然、快速而完全恢复。
晕厥可使人失健、致人受伤、诊治费钱,更重要的是它可能是猝死的前奏。一组数据显示,年龄在 15~35 岁之间的 162 位猝死病人中,25% 开始时表现为晕厥。
因此,我们必须对各种晕厥和类似晕厥做出鉴别诊断,再对其致猝死的危险性做出判断。以采取合适的防治措施,防止其复发、减少其损伤、避免发生猝死。
晕厥的常见病因是什么?
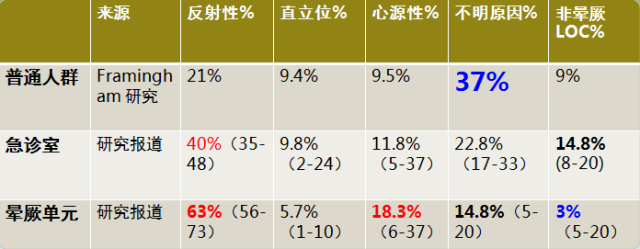
(最近临床研究晕厥的病因构成比)
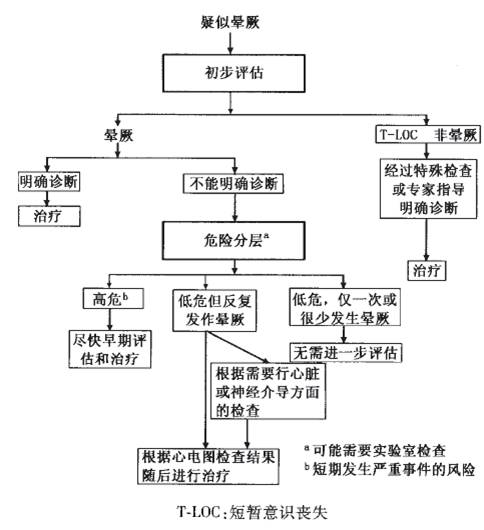
晕厥的诊断与评估
1. 首先应回答以下问题:
① 是否完全意识尚失(T-LOC)?
② LOC是否一过性伴快速起始和持续时间短?
③ 是否自发、完全恢复,不留后遗症?
④ 患者是否失去自我控制或肌紧张消失?
如果以上问题均明确,则晕厥可能性极大。如果≥1个不具备,要首先除外其他原因导致的LOC。
2. 晕厥诊断与评估流程:
3. 晕厥的病因诊断
① 晕厥发作前的情况(体位、活动等);
② 发作起始的伴随症状(恶心、呕吐、大汗等)、目击者看到的情况;
③ 发作结束时情况(胸痛、大小便失禁等);
④ 患者的背景资料(SCD家族史、既往病史、药物使用);
⑤ 平卧和立位血压测定,必要时颈动脉窦按摩(>40岁);
⑥ 23-50%患者经过初始评价能够明确病因。
4. 晕厥的危险性评估
——凡符合下列情况之一的是高危人群,需要强化评估或收住院诊治:
① 严重的结构性心脏病或冠心病(心力衰竭、左室射血分数较低及陈旧性心肌梗死),特别是胸痛与晕厥有关联;
② 猝死家族史 ;
③ 体位性晕厥:宫外孕破裂;消化道出血;血容量不足,例如呕吐、腹泻;
④ 高龄 ;
⑤ 其他:在吸入室内空气下,氧饱和度≤94%;电解质紊乱;严重贫血;BNP≥ 300pg/ml。
晕厥的7种检查方法
1. 颈动脉窦按摩试验 (CSM)
① 适用人群:40 岁以上,初步筛查未能明确诊断的晕厥患者;
② 可作为诊断颈动脉窦综合征的依据;
③ 左右两侧颈动脉窦依次进行 5~10 s 的按摩,患者取平卧位,若无阳性结果可再取立位 ;
④ 出现长达 3 s 以上的窦性停搏(心脏抑制型)或收缩压降低大于 50 mmHg(血管抑制型)可诊断颈动脉窦过敏;
⑤ 既往 3 个月内出现过短暂性脑缺血发作或卒中以及可及颈动脉杂音者(或颈动脉严重狭窄者)禁用。
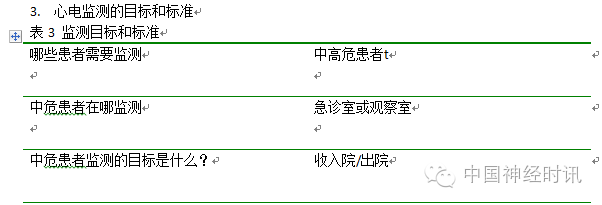
2. 心电监测(ECM)
① 心电图:5% 的阳性率;
② 医院内心电监护:存在致心律失常高危因素(如器质性心脏病)的晕厥患者 ,72 h 心电监护的诊出率也仅有 16% ;
③ 动态心电图:对预计 1 周内晕厥可能复发的患者应用;
④ 便携式心电记录器:可以被事件激活,识别能力有限,针对性患者阳性率 25% ;
⑤ 植入式心电记录器:植入式 Holter12- 36 个月,强烈怀疑晕厥为心律失常所致或反复晕厥受伤无其他原因,Holter 或便携式心电记录器无阳性发现时考虑应用。有创性,且价格较贵;
⑥ 心内电生理检查:结构性心脏病、心电图异常可能心律失常晕厥。
3. 主动站立测试(Active standing)
① 适用人群:所有初发晕厥尤其是老年以及服用降压药物或抗抑郁药物的患者进行;用于诊断直立性低血压 ;
② 直立后 30 秒到 3 分钟内出现血压收缩压降低大于 20 mmHg(高血压患者降低大于 30 mmHg)多见于成年人;
③ 站立即刻至 30 秒内血压下降达 30/20mmHg 以上, 多见于青年人;
④ 慢性直立性低血压:对有自主神经功能不全表现或相关基础疾病如糖尿病、帕金森病的患者,应延长体位改变后的血压监测时间 3 ~ 30 分钟。
4. 直立倾斜试验(Tilt Test)
① 适用人群:病史或现场描述怀疑而不能确诊的患者;用于老年人血管迷走性晕厥和意外跌倒事件的鉴别 ;
② 心动过缓和血压降低程度可分为心脏抑制型、血管抑制型和混合型,但直立倾斜试验所反映出的类型与实际晕厥时的类型并无必然联系;
③ 特异性 90%(无药物触发);
④ 不可重复性,直立倾斜试验不能用于治疗前后的疗效判断;
⑤ 下列情况慎用:缺血性心脏病、难以控制的高血压、左心室流出道梗阻、严重主动脉狭窄及有室性心律失常病史。
5. ATP 试验
① 适用人群:于心电图“正常”、无显著心脏疾病的不明原因的晕厥患者;
② 持续心电监护的条件下给予受试者 20 mg ATP 静脉注射,诱发的房室传导阻滞伴室性停搏时间持续 >6s,或可诱发的房室传导阻滞持续 >10 s 为异常;
③ 可靠性至今未得到公认,其结果与晕厥发生时植入式心电记录器的记录不符,不能成为起搏器植入的指征;
④ 最新研究显示,老年人不明原因晕厥,ATP 实验阳性,双腔起搏器植入可减少晕厥复发危险 75% (44-88);
⑤ 哮喘及其他严重呼吸系统疾病患者禁用。
6. 影像学检查
① 超声心动图是诊断结构性心脏病非常重要的技术,LVEF 在危险分层中有重要作用;
② 可明确少见的晕厥原因(如主动脉瓣狭窄、心房黏液瘤、心脏压塞等);
③ CTA 和 MRI 检查:主动脉夹层和血肿、肺栓塞、心脏肿瘤、心包和心肌疾病、冠状动脉先天畸形等。
7. 运动试验
① 适应证:运动过程中或运动后立即发生晕厥的患者;
② 发生在运动过程中的晕厥可能是心源性;
③ 运动之后发生的晕厥几乎都是由于反射机制所致;
④ 运动诱发的、心动过速之后的Ⅱ度和Ⅲ度房室传导阻滞表明病变可能位于房室结末端,并预示着可能进展为永久性房室阻滞。
晕厥的治疗方法
总原则:延长生存期、减少外伤、预防复发。
1. 反射性晕厥:
① 教育和让患者了解这一疾病的良性特点,尽量避免诱因;
② 物理治疗:一线治疗。等长压力对抗动作(PCM)、直立倾斜训练、下肢加压可有效减少血管迷走晕厥的发生;
③ 药物治疗:α受体激动剂米多君2.5mg,2~3次/日显著降低晕厥的发生率; 42岁以上,β阻断剂(美托洛尔)可有效抑制血管迷走晕厥;
④ 心脏起搏:价值有限,DDD对40岁以上心脏抑制为主的血管迷走神经性晕厥有效,而对血管抑制为主者无效。
2. 直立性低血压和不耐受综合征
① 教育和生活方式改变明显有效;
② 停用诱发自主神经异常性晕厥药物;
③ 扩容非常重要,无高血压患者可采取摄入足够的水和盐(2-3L/日水和10g食盐);
④ 弹力袜和PCM也有助于减轻症状;
⑤ 米多君(5-20mg, 每日三次)为慢性自主神经异常者首选药物,但并不是治愈,也不是对所有患者有效,但对部分患者很有效;
⑥ 部分患者对氟氢可的松(0.1-0.3mg,每日一次)亦有效。
3. 心律失常性晕厥
① 窦房结功能障碍:起搏治疗显著有效;
② 房室传导系统疾病:需起搏治疗;
③ 阵发性室上性、室性心动过速及房扑:首选导管消融;
④ 心衰、室速或室颤伴晕厥病因无法去除:植入ICD。
4. 结构性心脏病相关晕厥
① 治疗目标:预防晕厥复发,治疗基础疾病,以及降低SCD风险;
② 严重主动脉瓣狭窄或心房粘液瘤患者,手术为首选;
③ 急性心肺血管疾病患者,如肺栓塞、心肌梗死或心包填塞,应针对病理生理过程进行处理;
④ 肥厚性心肌病(合并或不合并左室流出道梗阻),应针对其心律失常进行相应处理,多数这类患者应植入ICD。
小结
1. 病史采集、体格检查等是晕厥病因初步诊断的基石。
2. 注意高危人群,有针对性的选择有价值的晕厥检查方法,提高晕厥的确诊率。
3. 教育患者、避免诱因、物理训练,治疗基础疾病,高危猝死病人 ICD 植入。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










值得学习
63
好详细阿!
64
够干
72
#晕厥#
34
#诊断与治疗#
29
好好好的总结
67
限制挺多
75
总结的很好,学习了
17
学习了,临床上经常遇到
30