JAMA Neurology:血浆 p-tau217 与 tau PET可用于预测AD
2022-01-08 网络 网络
血浆 p-tau217 与 tau PET 可能是临床前和前驱期 AD 富集的最佳选择。然而,血浆 p-tau217 在临床前 AD 中最为重要,而 tau PET 在前驱 AD 中更为重要
纵向tau PET常被用于研究针对AD更多上游事件的药物的作用,包括此类治疗是否可以减缓tau的积累和扩散,这可能表明除了靶向作用外,还有积极的临床效果。然而,要在临床试验中有效地使用纵向tau PET作为结果,在试验期间,对可能显示tau积累和扩散的个体进行富集是关键。这增加了检测治疗效果的统计能力。虽然样本富集可以基于基线生物标志物谱,但目前对于哪种生物标志物最能预测阿尔茨海默病 (AD) 不同临床阶段的纵向 tau 积累尚未达成共识。
Antoine Leuzy描述 AD 临床过程中的[18F]RO948 tau PET 纵向变化结果,并确定哪些生物标志物组合显示出与纵向 tau PET 和最佳优化临床试验丰富度的最强关联。研究结果发表在JAMA Neurology杂志。

这项纵向队列研究连续招募了淀粉样蛋白 β (Aβ) 阴性认知未受损 (CU) 参与者、Aβ 阳性 CU 个体、具有轻度认知障碍 (MCI) 的 Aβ 阳性个体和患有 AD 痴呆的个体。收集基线血浆和脑脊液Aβ42/Aβ40, tau蛋白苏氨酸-217 (p-tau217)、p-tau181和神经丝光磷酸化,磁共振成像,淀粉样PET和tau PET。
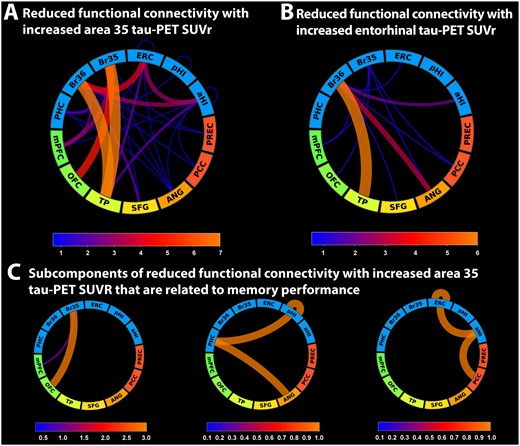
感兴趣区域的基线 tau PET 标准化摄取值比率 (SUVR) 和tau PET SUVR 年度百分比变化,使用数据驱动的方法结合聚类和基于事件的建模得出。用回归模型检查个体生物标志物与纵向 tau PET 之间的关联,并确定哪些组合最能预测纵向 tau PET。然后将这些组合输入到功效分析中,以检查它们作为富集策略的使用将如何影响模拟临床试验中的样本量。
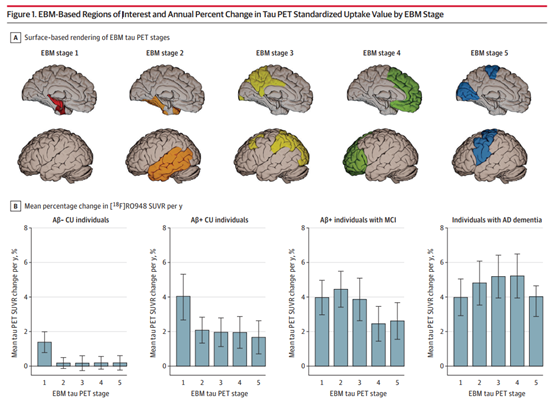
基于EBM的感兴趣区域和基于EBM阶段的Tau PET标准化吸收值的年变化百分比
在 343 名参与者中,平均 (SD) 年龄为 72.56 (7.24) 岁,157 名 (51.1%) 为女性。基于聚类/事件的建模方法确定了 5 个感兴趣的区域(阶段)。在 Aβ 阳性 CU 个体中,tau PET SUVR 的最大年度增幅出现在 I 期(内嗅皮层、海马和杏仁核;4.04% [95% CI,2.67%-5.32%])。在患有 MCI 和 AD 痴呆的 Aβ 阳性个体中,最大年度增幅出现在II 期(颞叶皮质区域;4.45% [95% CI,3.41%-5.49%])和 IV(某些额叶区域;5.22% [95 % CI,分别为 3.95%-6.49%])。在 Aβ 阴性 CU 个体和患有 MCI 的个体中,I期出现了中等变化 (1. 38% [95% CI,0.78%-1.99%] 和 1.80% [95% CI,0.76%-2.84%])。
当观察个体预测因子和显示变化最多的阶段的tau PET时,血浆 p-tau217(R2 = 0.27,P < 0.005)、tau PET(I 期基线 SUVR;R2 = 0.13,P < 0.05)和淀粉样蛋白 PET(R2 = 0.10,P < 0.05)与Aβ 阳性 CU 个体 I 期纵向 tau PET 显着相关。
在患有 MCI 的 Aβ 阳性个体中,血浆 p-tau217(R2 = 0.24,P < 0.005)和 tau PET(II 期基线 SUVR;R2 = 0.44,P < .001)与 II 期纵向 tau PET 显着相关。
对于功效分析组件,血浆 p-tau217 与 tau PET 导致Aβ 阳性 CU 个体样本量减少 43%(95% CI,34%-46%;P < 0.005) ,Aβ 阳性 MCI 个体样本量 减少68% (95% CI, 61%-73%; P < 0.001) 。
血浆 p-tau217 与 tau PET 可能是临床前和前驱期 AD 富集的最佳选择。然而,血浆 p-tau217 在临床前 AD 中最为重要,而 tau PET 在前驱 AD 中更为重要。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
32
#PE#
45
#PET#
47
#Tau#
39