Anesthesiology:“三低”状态与术后死亡率间存在显著相关性
2015-08-30 MedSci MedSci原创
临床数据显示,术后死亡率已不容小觑。许多研究发现,包括术中低血压,低脑电双频谱指数(BIS)值及低最小肺泡有效浓度(MAC)在内的围术期因素与术后死亡率存在显著相关性。研究人员将术中平均动脉压低于75mmhg,最小肺泡有效浓度低于0.8,脑电双频谱指数低于45同时发生的情况命名为“三低”状态。实际上,有关“三低”状态和术后死亡率相关性的研究已早有报道,但是并没有后续研究对其进行深入探讨。
临床数据显示,术后死亡率已不容小觑。许多研究发现,包括术中低血压、低脑电双频谱指数(BIS)值及低最小肺泡有效浓度(MAC)在内的围术期因素与术后死亡率存在显著相关性。研究人员将术中平均动脉压低于75mmHg,最小肺泡有效浓度低于0.8,脑电双频谱指数低于45同时发生的情况命名为“三低”状态。实际上,有关“三低”状态和术后死亡率相关性的研究已早有报道,但是并没有后续研究对其进行深入探讨。
为此,圣路易斯华盛顿大学医学院的研究人员通过一项观察性研究,对现有临床试验数据进行整合,进一步评估“三低”状态和术后死亡率之间的相关性。本次回顾性观察性研究共招募了13,198位来自三个临床试验组的患者:B-Unaware, BAG- RECALL, 和密歇根意识控制研究 。将术中“三低”状态多于15分钟的(可不连续)的患者,与将类似临床特征及并发症进行了严格控制的患者进行趋势性对比。使用多变量COX比例风险模型对持续性“三低”状态和术后死亡率的相关性进行评估。
结果显示,30天总体死亡率为0.8%,其中,“三低”组死亡率为1.9%,非“三低”组死亡率为0.4%。在对并发症进行匹配和调整后,“三低” 状态的累计持续时间和30及90天死亡率风险的增加呈显著的正相关。
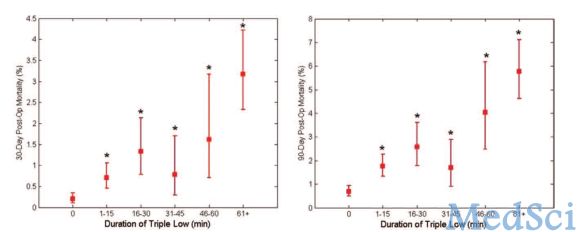
研究表明:“三低”状态和术后死亡率间存在着显著的相关性;同时,趋势性对比分析亦不能说明这种相关性只是偶然现象。
原始出处:
Willingham MD, Karren E,et al.Concurrence of Intraoperative Hypotension, Low Minimum Alveolar Concentration, and Low Bispectral Index Is Associated with Postoperative Death.Anesthesiology. 2015 Aug 12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








文章不错,值得拜读
62
#相关性#
39
#EST#
25
值得学习
124
这篇文章对围术期麻醉维持有重要指导意义
110
#ESI#
30
#术后死亡率#
33