全球BTK抑制剂亿珂®(伊布替尼)在中国获批
2017-10-17 佚名 MedSci
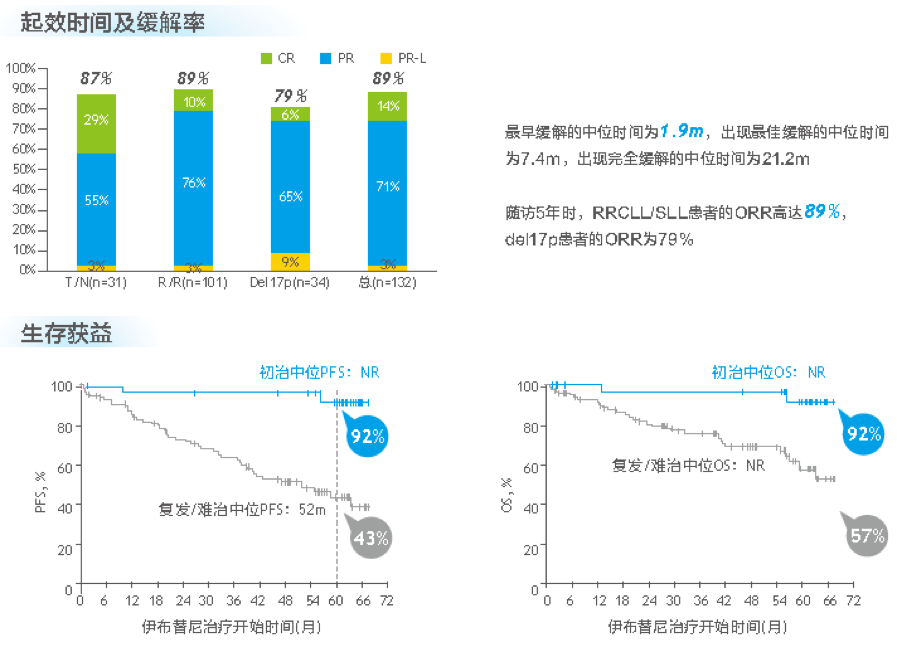
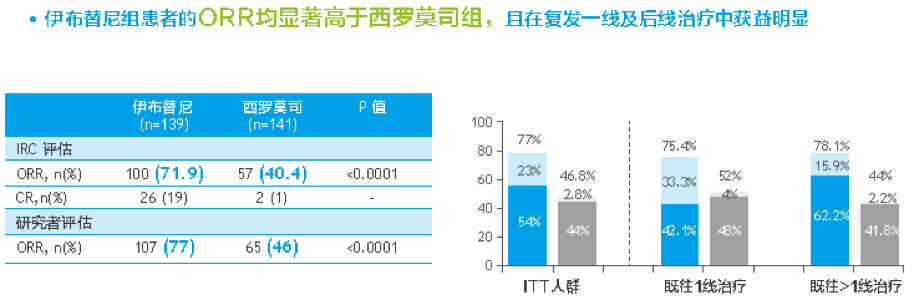
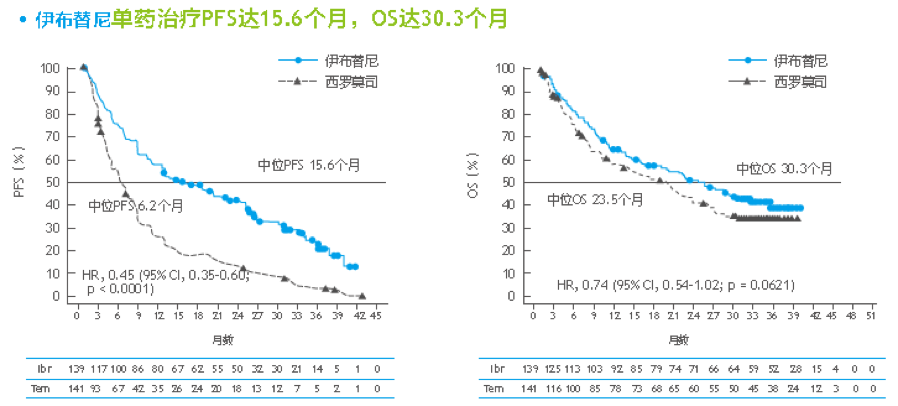
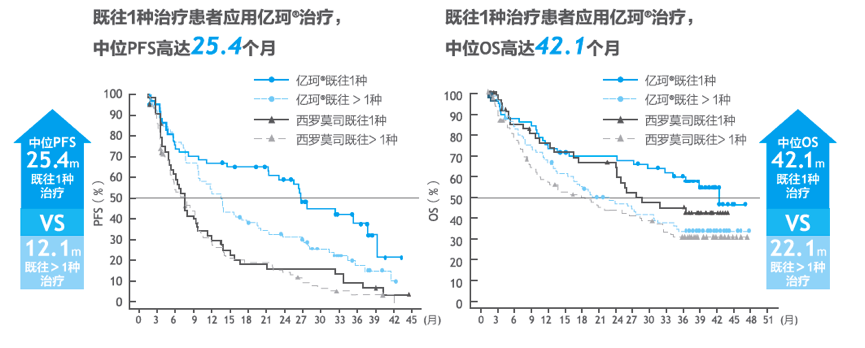
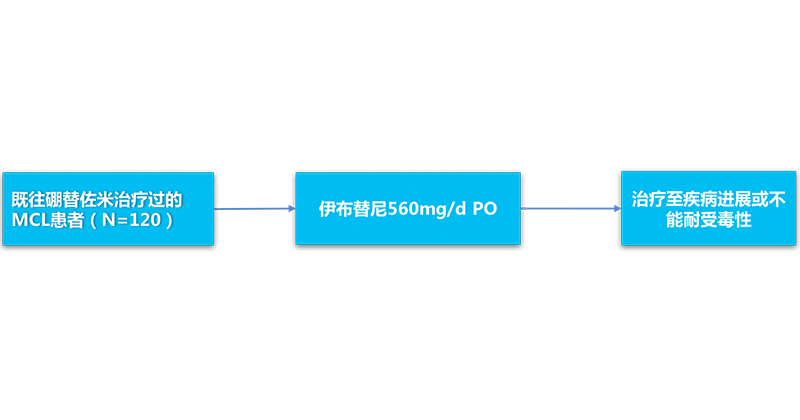
2017年8月24日,全球首个口服BTK抑制剂亿珂?(伊布替尼)正式获得中国食品药品监督管理总局(CFDA)批准,用于治疗慢性淋巴细胞白血病及套细胞淋巴瘤患者。亿珂?(伊布替尼)曾四次被FDA授予突破性药物认定,获得国际奖项“盖伦奖”,截止目前全球85个国家获批超过65000名患者受益,未来将开启中国B细胞淋巴瘤治疗的新纪元!BTK抑制剂的发现发展之旅-新型靶向药物的诞生据报道,1999年合成了首

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
19
#亿珂#
35
#伊布替尼#
35
#BTK抑制剂#
35
#BTK#
23