Lancet Oncol:科学家揭开癌症风险的复杂遗传奥秘
2016-08-08 佚名 生物谷
图片来源:medicalxpress.com癌症是一种机体多基因疾病,然而目前研究者们并不清楚我们机体的遗传组成如何影响患癌风险。近日,刊登在国际杂志The Lancet Oncology上的一项研究报告中,来自澳大利亚的研究人员通过研究深入理解了肉瘤的遗传学风险,研究人员对1000多名肉瘤患者进行了一项里程碑式的研究,揭开了引发癌症的多个新型的遗传风险因素,研究者指出,对于任何一种癌症类型而言
图片来源:medicalxpress.com
癌症是一种机体多基因疾病,然而目前研究者们并不清楚我们机体的遗传组成如何影响患癌风险。近日,刊登在国际杂志The Lancet Oncology上的一项研究报告中,来自澳大利亚的研究人员通过研究深入理解了肉瘤的遗传学风险,研究人员对1000多名肉瘤患者进行了一项里程碑式的研究,揭开了引发癌症的多个新型的遗传风险因素,研究者指出,对于任何一种癌症类型而言,携带两种或较多的遗传突变往往会增加个体的患癌风险。
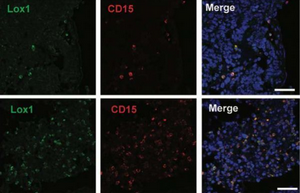
肉瘤是一种影响年轻人的结缔组织癌症,同时在澳大利亚其也是引发儿童和年轻人因疾病死亡的三大原因之一,而且肉瘤患者往往患第二种癌症的风险较高。这项和癌症风险相关连的研究是由澳大利亚的研究人员领导的国际肉瘤家族研究(ISKS)所进行的,研究者利用一种由72个基因组成的“基因检测盘”对每一个参与者机体中的突变进行检测,随后他们在一系列新型基因中鉴别出了可增加个体患肉瘤风险的特殊突变,包括基因ERCC2, ATR, BRCA2和ATM。
更重要的是,携带两个基因突变的个体患肉瘤的风险要明显高于仅携带一个基因突变的个体,如果个体携带有三个或更多基因突变,其患癌风险会更高。研究者David Thomas说道,这项研究中我们首次发现,对于任何类型的癌症而言,我们或许都可以测定多种罕见遗传突变对其患癌风险的效应。截止到目前为止,由于我们局限于单基因的思考,比如我们会告诉患者,携带BRCA1突变往往会增加患乳腺癌的风险,或者如果p53基因发生突变的话,其患肉瘤及其它癌症的风险就会增加等等。这项研究就指出,癌症风险的蓝图远比我们想象中要复杂得多,如今我们可以看到,通过结合多种基因的效应或许就会增加个体患肉瘤的风险,而且个体携带的突变越多,其出现癌症的表现就越早。这些之前看不到的效应至少有p53基因突变所产生的效应那么大,而p53基因突变被认为是引发肉瘤的主要原因。
对于一系列癌症而言,比如乳腺癌和肠癌,个体的患癌风险往往是由遗传自父母亲的基因所决定的;研究者指出,大约有一半的参与者都携带有至少一种明显的促癌突变,而且几乎有四分之一的个体携带着至少两个基因突变,而这就再次说明肉瘤风险的获得从很大程度上来讲是遗传自父母亲。Thomas教授说道,这项研究对于后期开发个体化癌症疗法提供了一定希望;理解增加个体患癌的遗传驱动子或可帮助我们理解如何更好地治疗患癌个体的病情,对于我们已经研究的三分之一的个体而言,其所携带的基因突变往往可以给我们提供重要的信息,即个体如何有规律地进行疾病监测和治疗。
举个例子,ERCC2基因主要参与对化疗制剂的解毒作用,因此对于携带ERCC2突变的患者而言,化疗或许并不是一种最为合适的疗法。而对于携带BRCA2的个体而言,其患肉瘤的风险同患乳腺癌、卵巢癌的风险一样,而这或许就可以帮助研究者对患者进行新型疗法的治疗。
研究者后期还需要进行更多研究来揭示,如何利用机体风险遗传信息来改变治疗癌症患者的方法,研究者知道的越多,就越能精确地将患者同最合适的疗法进行匹配来治疗疾病;本文研究为科学家们后期调查整个基因组,寻找增加机体肉瘤风险的遗传突变提供了一定线索,研究者希望后期可以鉴别出一系列能够影响个体患恶性癌症的突变。
原始出处
Mandy L Ballinger, PhD*, David L Goode, PhD*, Prof Isabelle Ray-Coquard, MD, Paul A James, MBChB, Gillian Mitchell, PhD, Eveline Niedermayr, BSc, Prof Ajay Puri, MS.et.al.Monogenic and polygenic determinants of sarcoma risk: an international genetic study.Lancet Oncol.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
20
#Lancet#
28
很好,不错,以后会多学习
46
很好,不错,以后会多学习
64
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
63
继续学习
50
继续关注
67