共识易览:类风湿关节炎的慢病管理如何进行?
2016-04-19 指南君 中华风湿病学杂志
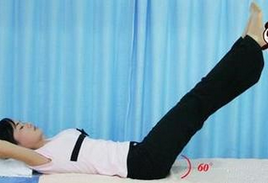
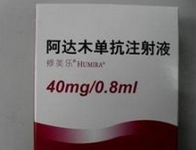
类风湿关节炎(RA) 是一种自身免疫性、系统性的慢性炎症性多关节炎,目前尚无治愈方法。慢病管理(CDM)是指组织慢性病专业医生、护士、药师、康复科医师、精神科医师、营养师等作为一个医疗团队,为慢性病患者提供全面、连续、主动的管理,从而达到促进健康、延缓疾病进程和降低伤残率、降低医药费用的一种科学管理模式。 《类风湿关节炎慢病管理专家共识》包含12 条建议,建议的推荐强度为A到D,具有较高
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











挺不错的
126
#关节炎#
29
#类风湿#
20
#风湿关节炎#
26
文章高大上
126
值得关注
75