NEJM:支架内血栓和支架内再狭窄
2017-01-03 小燕子 医课室
研究指出,支架内血栓发生率 1 年内< 1%,随后每年发生率为 0.2%~0.4%。支架内再狭窄的发生率约为 5%。近日,来自德国慕尼黑大学的 Robert A 教授在新英格兰医学杂志上发表了一篇有关支架内血栓形成和支架内再狭窄的综述,小编在此跟大家分享一下。即使围手术期的抗栓治疗、抗血小板药物的革新、新型药物洗脱支架的使用,使短期到中期内支架植入患者预后明显提高,但心脏支架并不能一劳永
研究指出,支架内血栓发生率 1 年内< 1%,随后每年发生率为 0.2%~0.4%。支架内再狭窄的发生率约为 5%。
近日,来自德国慕尼黑大学的 Robert A 教授在新英格兰医学杂志上发表了一篇有关支架内血栓形成和支架内再狭窄的综述,小编在此跟大家分享一下。
即使围手术期的抗栓治疗、抗血小板药物的革新、新型药物洗脱支架的使用,使短期到中期内支架植入患者预后明显提高,但心脏支架并不能一劳永逸地解决冠心病血管堵塞问题,还可能在支架植入后形成血栓和再狭窄。
研究指出,支架内血栓发生率 1 年内< 1%,随后每年发生率为 0.2%~0.4%。支架内再狭窄的发生率约为 5%。
1 年内 < 1%?概率挺小的嘛?即使概率不高,但支架内血栓一旦形成,在临床上发生心脏猝死,急性心肌梗死或不稳定型心绞痛等,其中引发的血栓形成段的抬高型心肌梗死,死亡率可高达 20%-40%!
砸锅卖铁还冒着生命危险放个支架,血栓照样会形成,人生真的好艰难,有木有?
那么,支架内血栓是怎么形成的呢?

以支架植入后30 天为分界线,支架内血栓形成(ST)分为两类,即早期支架内血栓形成和迟发支架内血栓形成。
到底是什么令血栓在支架植入30天内形成呢?高估狭窄程度或者低估血管直径而导致支架直径选择不当(好的外科医生就得如同好的裁缝那样精准),以及支架植入部位血管受损、TIMI 血流受损、支架损伤近端或远端残余狭窄、左室收缩功能减退、ADP 拮抗剂治疗失败等,均能导致早期支架内血栓形成。另外,过早弃疗,即早期中断抗血小板治疗(支架植入后 30 天内),也会导致血栓的形成。
同样的,迟发支架内血栓形成与支架大小不合适、植入部位不当也相关,以及左室收缩功能受损、糖尿病和ADP 拮抗剂治疗失败均会增加迟发支架内血栓形成的风险。
支架类型也是其中一个影响因素,有研究指出,西罗莫司和紫杉醇涂层支架会增加迟发支架内血栓形成风险,其机制可能与迟发动脉修复、内皮损伤、持续性纤维蛋白沉积、血管壁炎症等相关。具有更薄的支架支杆、更合适的多聚物涂层以及少量的西罗莫司等药物涂层的新一代药物洗脱支架可更好改善血栓形成的问题。
双联抗血小板治疗预防支架内血栓形成
研究表明,在裸支架植入的患者中,双联抗血小板治疗比抗凝治疗效果好。因此,专家建议PCI术后进行双联抗血小板治疗。 而双抗治疗的时间长短很关键,普遍的双抗治疗时间窗为 6 个月到 30 个月,目前专家建议治疗时间至少持续12个月, 时间越长,支架内血栓形成的发生率和总体心血管事件的发生率越低,但可能会增加出血事件的发生。
那么,抗血小板治疗药物哪个强?研究表明,ADP 受体拮抗剂在减少支架内血栓形成发生率上优于氯吡格雷。尤其是经静脉注射 ADP 受体拮抗剂,可以减少支架植入后急性期支架内血栓形成。
祸不单行——支架内再狭窄(ISR)
可谓祸不单行,植入支架后,这厢血栓,那厢就狭窄。

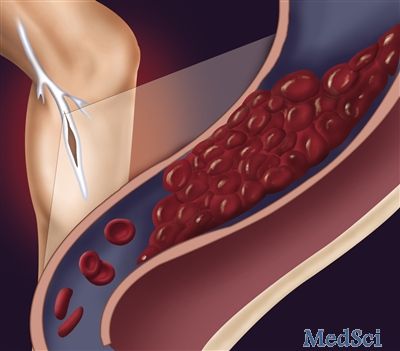
PCI 术后血管壁损伤引起相关炎症反应,促使成纤维母细胞和平滑肌细胞增生,是发生支架内再狭窄的机制。主要分为5步:急性或亚急性斑块脱落;血管壁弹性回缩;血管重塑;内膜增生;支架内动脉粥样硬化。
血管造影发现植入支架后管腔直径再次狭窄 > 50% 可定义为支架内再狭窄。血管内成像可提供三维影像,如若发现新出现管腔之间狭窄 > 75% 则提示支架内再狭窄。除此之外,支架内再狭窄还包括伴随需要再次治疗的临床症状如缺血症状发作。
较小的管腔直径、支架整体长度、损伤处形态学、糖尿病史、既往搭桥手术病史均是再狭窄的独立危险因素。
植入裸金属支架发生支架内再狭窄的风险为 30%,其病理过程主要是造成内膜增生,大量平滑肌细胞增殖及细胞外基质分泌增加。
植入药物洗脱支架后发生率可降至 15% 以下,药物洗脱支架的病理特点主要是内膜增生和相对较少的平滑肌细胞。同时在药物洗脱支架再狭窄中,新生动脉粥样硬化反而更为常见。
药物洗脱支架管腔狭窄主要发生在术后 6 至 8 个月的时间窗内及 2 年后。这可能与动脉内皮延迟愈合相关。除此之外,研究也表明药物洗脱支架相关的暂时性再狭窄可能较植入裸金属支架更易清除。
治疗方法:重新植入新一代的药物洗脱支架或者药物涂层球囊
支架内再狭窄的发生对 PCI 术后长期预后影响极大,可能会引起心绞痛、心肌梗死,约 20% 的患者可能存在急性心肌酶阳性。患者一般都需要再次行介入治疗,重新植入新一代的药物洗脱支架或者药物涂层球囊。
春风吹又生:新生动脉粥样硬化
支架内新发动脉粥样硬化斑块既是新生动脉粥样硬化,其过程为:早期泡沫化的巨噬细胞浸润;持续性斑块形成;坏死脂质核心形成。
药物洗脱支架可引起内皮细胞结构和功能受损,使内皮愈合延迟,新生动脉粥样硬化容易形成。所以新发动脉粥样硬化斑块在药物洗脱支架中发生更早,比例更高,而在植入裸金属支架中也可观察到这种情况,但相对药物洗脱支架,形成斑块的时间晚些。
运用OCT 检查手段可以监测支架内新生动脉粥样硬化的情况。
革命之路:生物可吸收支架

生物可吸收支架(BRS)可消除支架内血栓形成和再狭窄的风险,是 PCI 治疗史上的一次革新。
相比传统的支架,BRS好处不少:如恢复支架植入段血管的收缩功能、增加管腔直径,进一步缓解心绞痛。
虽然,BRS 在短期随访内其临床效果是令人满意的,再狭窄发生率明显降低,但其植入操作过程较为复杂,也存在早期支架内血栓形成的发生风险,所以革命之路绝不是一马平川的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#支架内再狭窄#
31
#支架内血栓#
35
求这篇新英格兰杂志发表的文章名称
55
#再狭窄#
48
谢谢,学习一下
61
感谢分享,学习了
54