Blood:CCND1和STAT3参与套细胞淋巴瘤中SOX11的表达调控
2019-01-02 MedSci MedSci原创
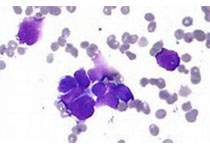
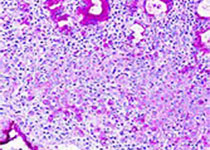
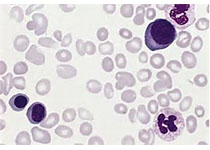
中心点:CCND1与HDAC1/2结合,阻碍其招募至SOX11启动子,从而增强组蛋白乙酰化和SOX11的转录。STAT3通过与SOX11基因的启动子和增强子直接相互作用来抑制SOX11的转录。摘要:神经转录因子SOX11在经典套细胞淋巴瘤(MCL)中常高表达,但在较为惰性的MCL亚型中不表达。虽然SOX11是该难治疗的恶性肿瘤的一个重要的预后标志物,但其异常表达的机制还基本不明确。Atish Mo
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CCND#
51
#表达调控#
31
#细胞淋巴瘤#
37
#STAT3#
49
学习谢谢分享
77
了解一下
64
好
79