ADAURA III期临床研究结果公布:奥希替尼治疗中枢神经系统转移可改善无病生存期
2020-09-22 网络 网络
一项基于获得阳性结果的III期ADAURA临床研究的预设探索性分析显示,阿斯利康公司的泰瑞沙在对接受过完全肿瘤切除术的早期
一项基于获得阳性结果的III期ADAURA临床研究的预设探索性分析显示,阿斯利康公司的泰瑞沙(化学名:奥希替尼Osimertinib,商品名:泰瑞沙Tagrisso)在对接受过完全肿瘤切除术的早期(IB、II和IIIA期)表皮生长因子受体突变(EGFRm)非小细胞肺癌(NSCLC)患者的辅助治疗中,可带来具有临床意义的中枢神经系统(CNS)无病生存期(DFS)改善。
虽然近30%的非小细胞肺癌患者由于早期得到诊断,可以接受以治愈为目的的手术,但疾病复发在这些早期患者中仍然常见。中枢神经系统复发,即当癌症扩散到脑部,是EGFR突变非小细胞肺癌的常见并发症,而出现此类复发的患者通常预后非常差。
研究结果已于9月19日在2020欧洲肿瘤内科学会(ESMO)线上年会的主席论坛环节发布(摘要编号:LBA1),研究的主要结果也同步发表于《新英格兰医学杂志》。
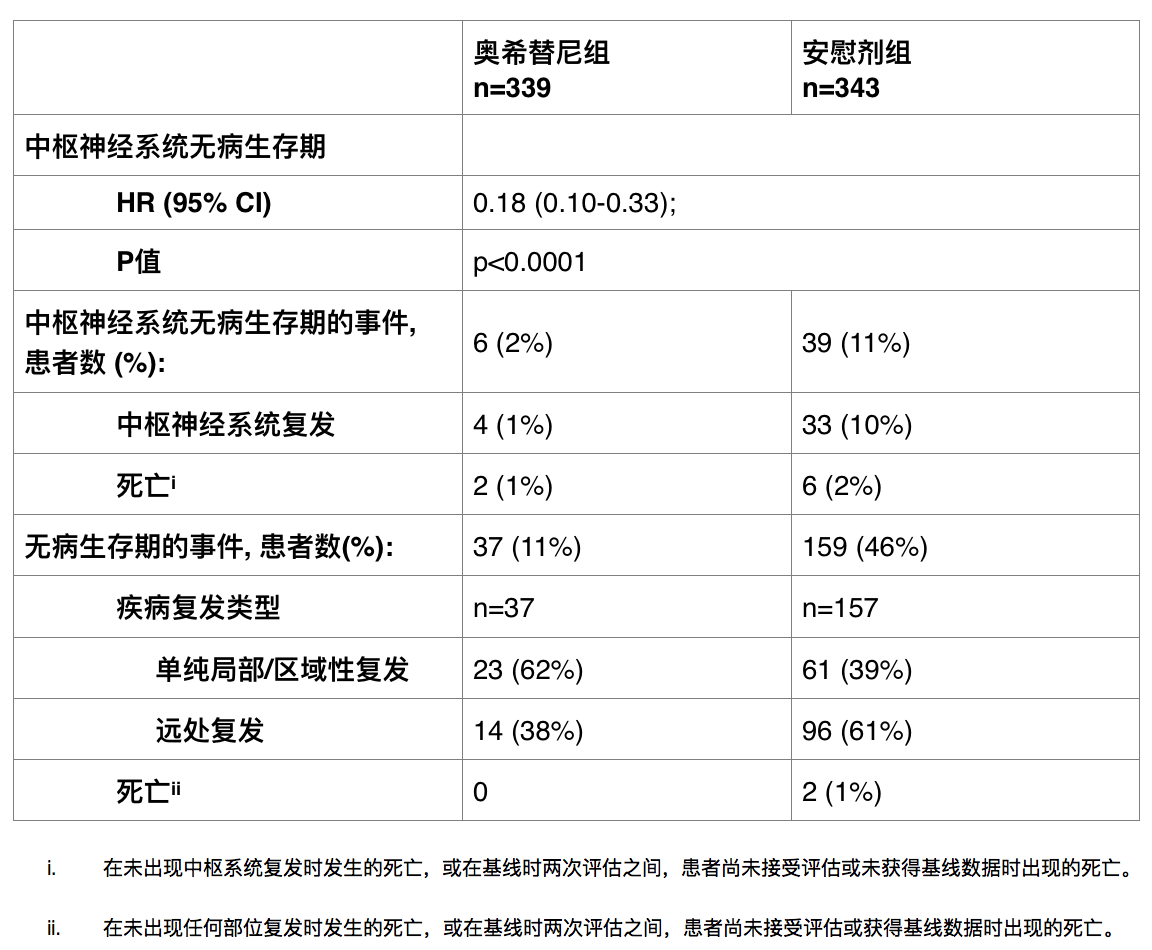
分析结果提示,奥希替尼辅助治疗组较安慰剂组有更少患者出现了复发或死亡 (11% vs. 46%)。在已出现疾病复发的患者中,奥希替尼组中有38%的患者出现了转移性复发,而安慰剂组为61%。奥希替尼可显著降低中枢神经系统复发或死亡风险82%(风险比[HR] 0.18;95%置信区间[CI] 0.10-0.33;p<0.0001)。两组均未达到中位中枢神经系统无病生存期 (CNS DFS)。
一项事后分析提示,在既往未出现其他部位复发的患者中,接受奥希替尼治疗的患者18个月时出现脑部疾病复发的估算几率低于1%,而安慰剂组为9%。主要研究终点-II期和IIIA期患者的无病生存期,奥希替尼辅助治疗降低了83%疾病复发或死亡的风险(HR 0.17; 95% CI 0.12-0.23; p<0.0001)。
Masahiro Tsuboi博士是日本东部国立肿瘤中心医院胸外及肿瘤科主任并且是ADAURA研究主要研究者,他表示:“现在应该改变早期EGFR突变肺癌手术后停止治疗这一观念了, 因为即使在辅助化疗后,复发率依然很高。此次发布的最新数据显示了低复发率 - 尤其是脑部复发率,以及显著的无病生存期获益,充分显示奥希替尼可延长患者的无肿瘤生存期。”
阿斯利康全球执行副总裁,肿瘤研发部负责人José Baselga表示:“一旦肺癌扩散至脑部,患者通常预后极差。我们目前看到,奥希替尼具有穿透血脑屏障的能力,数据进一步验证了奥希替尼在脑转移治疗进展中的有效性。这次优异的新数据表明奥希替尼可预防早期EGFR突变肺癌患者的脑部转移,并进一步证明奥希替尼为早期EGFR突变肺癌的治疗带来了真正革命性的进步。正如全球在治疗转移性肿瘤的那样,奥希替尼也应当成为辅助治疗的标准治疗。“
奥希替尼在本研究中显示的安全性和耐受性与之前对于转移性EGFR突变非小细胞肺癌的研究结果一致。经研究人员评估,奥希替尼组中任何原因导致的大于等于3级不良事件发生率为10%,而安慰剂组中为3%。
奥希替尼目前尚未在任何国家获批用于辅助治疗。奥希替尼于2020年7月获得了突破性疗法认定,作为接受过以治愈为目的完全肿瘤切除的早期EGFR突变非小细胞肺癌患者的辅助治疗。奥希替尼已在美国、日本、中国及欧盟等全球多地获批用于局部晚期或转移性EGFR突变非小细胞肺癌的一线治疗,以及局部晚期或转移性EGFR T790M突变非小细胞肺癌的治疗。
肺癌
肺癌是男性和女性癌症死亡的主要原因,约占所有癌症死亡人数的五分之一。6 通常,肺癌分为非小细胞肺癌(NSCLC)和小细胞肺癌(SCLC),其中80%-85%为非小细胞肺癌。7 大部分NSCLC患者在确诊时已是晚期,其中只有大约25-30%的患者在确诊时有机会接受手术治疗。
美国和欧洲约有10-15%的非小细胞肺癌患者存在EGFR突变(EGFRm),而亚洲患者中该比例高达30-40%。11-13 这些患者对表皮生长因子受体酪氨酸激酶抑制剂(TKI)的治疗特别敏感,这种抑制剂可阻断驱动肿瘤细胞生长的信号传导途径。
ADAURA临床研究
ADAURA是一项随机、双盲、安慰剂对照的全球III期临床试验,入组682例IB、II、IIIA EGFRm阳性非小细胞肺癌患者接受辅助治疗,患者既往接受过完全肿瘤切除和辅助化疗。患者接受口服奥希替尼80mg,每日一次,或安慰剂,持续3年或直至疾病复发。
该试验在全球200多个中心开展,涉及20多个国家包括美国、欧洲、南美、亚洲和中东。主要研究终点是II期和IIIA期患者的DFS,关键的次要研究终点是IB期、II期和IIIA期患者的DFS。数据发布最初预计在2022年进行。试验将继续评估总生存期(OS)数据。
References
1. Cagle P, et al. Lung Cancer Biomarkers: Present Status and Future Developments. Archives Pathology Lab Med. 2013;137:1191-1198.
2. Le Chevalier T. Adjuvant Chemotherapy for Resectable Non-Small-Cell Lung Cancer: Where is it Going? Ann Oncol. 2010;21:196-8.
3. Datta D, et al. Preoperative Evaluation of Patients Undergoing Lung Resection Surgery. Chest. 2003;123: 2096–2103.
4. Rangachari, et al. Brain Metastasesin Patientswith EGFR-Mutatedor ALK-RearrangedNon-Small-Cell LungCancers. LungCancer. 2015;88,108–111.
5. Ali A, et al. Survival of Patients with Non-small-cell Lung Cancer After a Diagnosis of Brain Metastases. CurrOncol. 2013;20(4):e300-e306.
6. World Health Organization. International Agency for Research on Cancer. Lung Fact Sheet. Available at http://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf. Accessed September 2020.
7. LUNGevity Foundation. Types of Lung Cancer. Available at https://www.lungevity.org/about-lung-cancer/lung-cancer-101/types-of-lung-cancer. Accessed September 2020.
8. Pignon et al. Lung Adjuvant Cisplatin Evaluation: A Pooled Analysis by the LACE Collaborative Group. J Clin Oncol 2008;26:3552-3559.
9. Sethi S, et al. Incidental Nodule Management – Should There Be a Formal Process?. Journal of Thorac Onc. 2016:8;S494-S497.
10. LUNGevity Foundation. Screening and Early Detection. Available at: https://lungevity.org/for-patients-caregivers/lung-cancer-101/screening-early-detection#1. Accessed September 2020.
Szumera-Ciećkiewicz A, et al. EGFR Mutation Testing on Cytological and Histological Samples in 11. Non-Small Cell Lung Cancer: a Polish, Single Institution Study and Systematic Review of European Incidence. Int J Clin Exp Pathol. 2013:6;2800-12.
12. Keedy VL, et al. American Society of Clinical Oncology Provisional Clinical Opinion: Epidermal Growth Factor Receptor (EGFR) Mutation Testing for Patients with Advanced Non-Small-Cell Lung Cancer Considering First-Line EGFR Tyrosine Kinase Inhibitor Therapy. J Clin Oncol. 2011:29;2121-27.
13. Ellison G, et al. EGFR Mutation Testing in Lung Cancer: a Review of Available Methods and Their Use for Analysis of Tumour Tissue and Cytology Samples. J Clin Pathol. 2013:66;79-89.
14. Cross DA, et al. AZD9291, an Irreversible EGFR TKI, Overcomes T790M-Mediated Resistance to EGFR Inhibitors in Lung Cancer. Cancer Discov. 2014;4(9):1046-1061.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#III期临床研究#
41
#结果公布#
27
#III#
31
#I期临床#
32
#II期临床研究#
30
#研究结果#
35
#ADA#
30
#神经系统#
37
#生存期#
22
#II期临床#
28