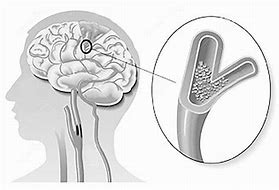
Neurology:SAH 后早期脑损伤与早期播散去极化有关
2019-02-23 杨中华 脑血管病及重症文献导读
动脉瘤破裂后,脑实质损害决定了患者的预后。初期的全面缺血会引起弥漫性全脑水肿(global cerebral edema,GCE)和不良预后。在介入前的 CT 扫描中,脑出血(ICH)周围往往环绕着局灶损害。早期或延迟局灶性损害更常见于被血液填充的脑沟和脑裂周围的皮质。在传统的病理文献中,这些损害被称为『局灶性贫血坏死(“focal anemic necroses)』,在 CT 上表现为明显的低密
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Neurol#
26
#播散去极化#
0
#损伤#
22
#SAH#
28
学习了很有用不错
55