Cancer:纳武单抗联合伊匹单抗治疗晚期肾细胞癌伴有脑转移患者的安全性和有效性(CheckMate 920)
2022-04-07 yd2015 MedSci原创
研究表明,Nivolumab(那武利尤单抗)联合ipilimumab(伊匹木单抗)治疗晚期肾细胞癌伴有脑转移患者有效且毒性可耐受。
CheckMate 920是一项前瞻性、非随机、开放标签、多队列、3b/4期临床试验,评估Nivolumab(那武利尤单抗)联合ipilimumab(伊匹木单抗)治疗既往未经治疗的晚期肾细胞癌(aRCC)或转移性RCC患者的疗效。患者被分配到4个队列:主要透明细胞RCC (ccRCC)伴KPS ≧70%(队列1)、nccRCC伴KPS ≧70%(队列2)、cc/ ncccc伴无活动性脑转移和≧KPS 70%(队列3)以及cc/ nccRCC伴KPS 50% ~ 60%(队列4)。Cancer杂志上报告了队列3的研究成果。
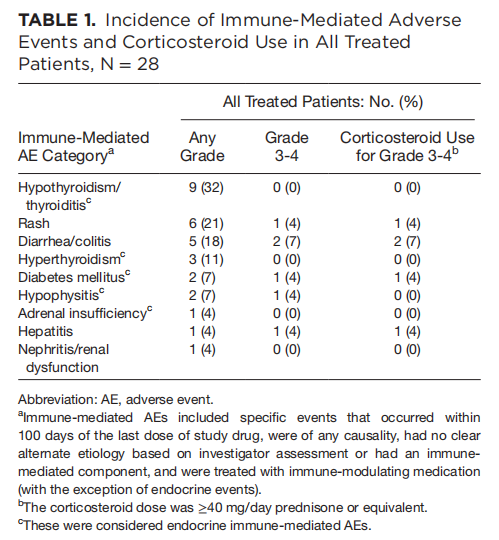
主要终点是最后一次给药后100天内≧3级免疫介导不良事件(imAEs)的发生率。关键的次要终点是无进展生存期和客观缓解率(均由研究者确定)。探索性终点包括总体生存率等。
队列3中28例脑转移患者接受NIVO治疗(所有患者均已接受治疗)。病人的平均年龄是60岁(范围,38 - 87年),86% (n = 24)是男性,100% (n = 28)患者的KPS ≧70%, 64% (n = 18)患者IMDC风险评分为中度风险。在可评估肿瘤PD-L1表达水平的患者中,26% (n = 7)的PD-L1表达水平≧1%。
在最少24.5个月的研究随访后,所有患者停止治疗。在所有接受治疗的患者(N = 28)中,最常见的停药原因是疾病进展(N = 12;43%)和研究药物毒性(n = 8;29%)。
无5级imAEs(死亡)发生。最常见的3级和4级imAEs为腹泻/结肠炎(n = 2;7%)和垂体炎、皮疹、肝炎和糖尿病(各1例;4%)。
客观缓解率(ORR)为32% (95% CI, 14.9%-53.5%),无患者获得完全缓解,8例(32%)获得部分缓解,10例(40%)病情稳定,6例(24%)病情进展。存在或不存在肉瘤样特征的患者的ORR分别为67% (95% CI, 9%-99%)和27% (95% CI, 11%-50%)。基线肿瘤PD-L1表达水平<1%或≧1%的患者的ORR分别为37% (95% CI, 16%-62%)和20% (95% CI, 1%-72%)。

中位TTR为2.8个月(范围2.4-3.0个月)。中位DOR为24.0个月(范围3.9 - 32.7+月)。
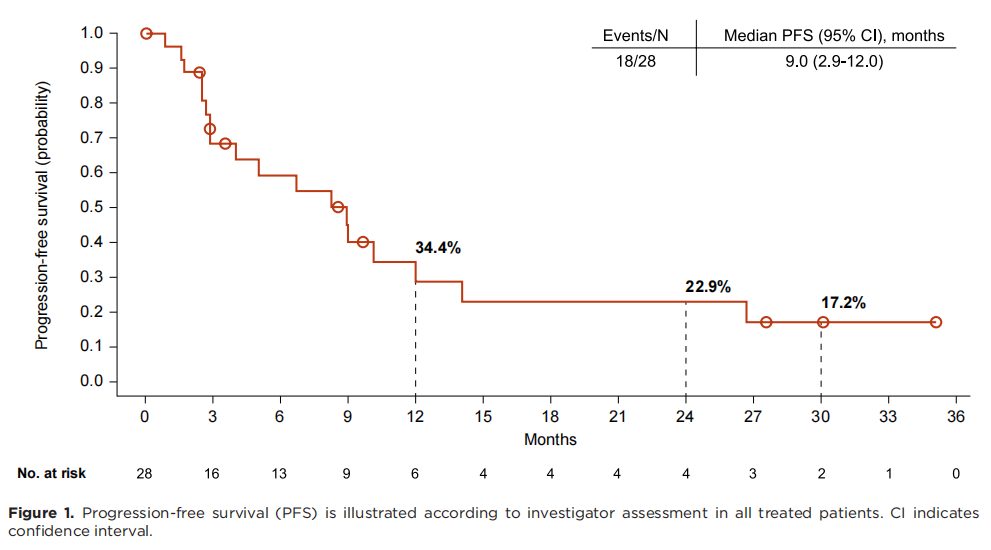
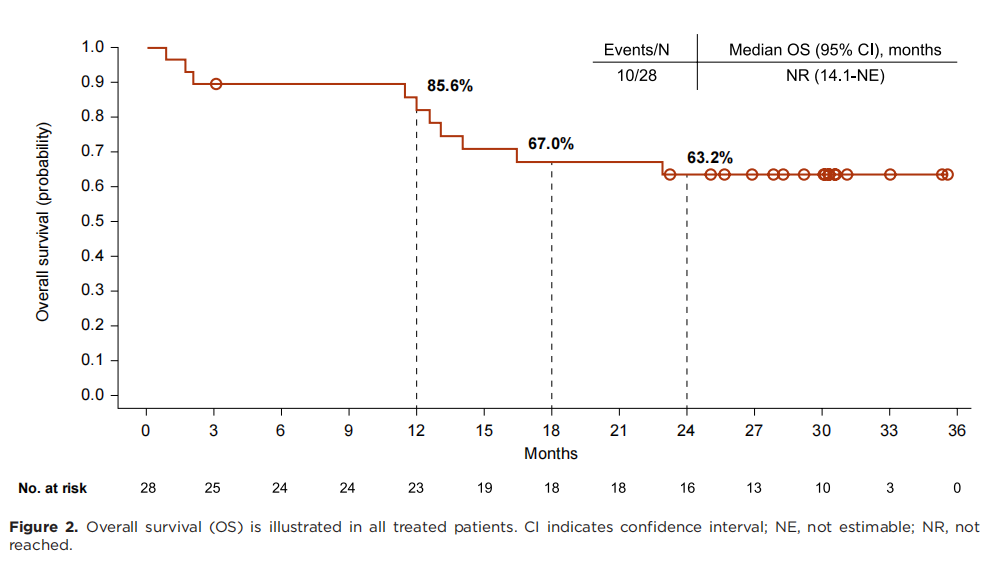
所有患者的中位PFS为9.0 个月(95% CI, 2.9-12.0)。而中位OS尚未达到(95% CI, 14.1-无法评估)。 12、18和24个月的OS率分别为85.6% (95% CI, 66.0%-94.3%), 67.0% (95% CI, 46.1%-81.3%), 和63.2% (95% CI, 42.4%-78.3%)。
综上,研究表明,Nivolumab(那武利尤单抗)联合ipilimumab(伊匹木单抗)治疗晚期肾细胞癌伴有脑转移患者有效且毒性可耐受。
原始出处:
Emamekhoo H, Olsen MR, Carthon BC, Drakaki A, Percent IJ, Molina AM, Cho DC, Bendell JC, Gordan LN, Rezazadeh Kalebasty A, George DJ, Hutson TE, Arrowsmith ER, Zhang J, Zoco J, Johansen JL, Leung DK, Tykodi SS. Safety and efficacy of nivolumab plus ipilimumab in patients with advanced renal cell carcinoma with brain metastases: CheckMate 920. Cancer. 2022 Mar 1;128(5):966-974. doi: 10.1002/cncr.34016. Epub 2021 Nov 16. PMID: 34784056.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Checkmate#
42
#脑转移患者#
45
#细胞癌#
30
#安全性和有效性#
33
#晚期肾细胞癌#
37