JAMA Netw Open:糖尿病患者想要更好的管理体重和血糖,那就试试智能手机应用程序吧
2021-06-14 MedSci原创 MedSci原创
生活方式干预在糖尿病管理中是有效的,管理健康数据和饮食及运动计划的智能手机应用程序越来越受欢迎。然而,有关基于智能手机干预措施在亚洲成人2型糖尿病患者中的有效性证据有限。
生活方式干预在糖尿病管理中是有效的,管理健康数据和饮食及运动计划的智能手机应用程序越来越受欢迎。然而,有关基于智能手机干预措施在亚洲成人2型糖尿病患者中的有效性证据有限。

pixabay
近日,发表在JAMA Netw Open杂志的一项研究显示,与常规护理相比,基于智能手机的生活方式干预在降低亚洲 2 型糖尿病成人的体重和血糖方面更有效,支持在生活方式干预中使用应用程序。
在这项研究中,研究人员对来自新加坡多个初级保健中心进行的 305 名患有 2 型糖尿病且体重指数 (BMI) 为 23 或更高的成年人进行试验,这些参与者均具有良好的英语读写能力和使用智能手机的能力。最终纳入204 名符合要求的参与者,并随机分配干预组(n=99)或对照组(n=105)。
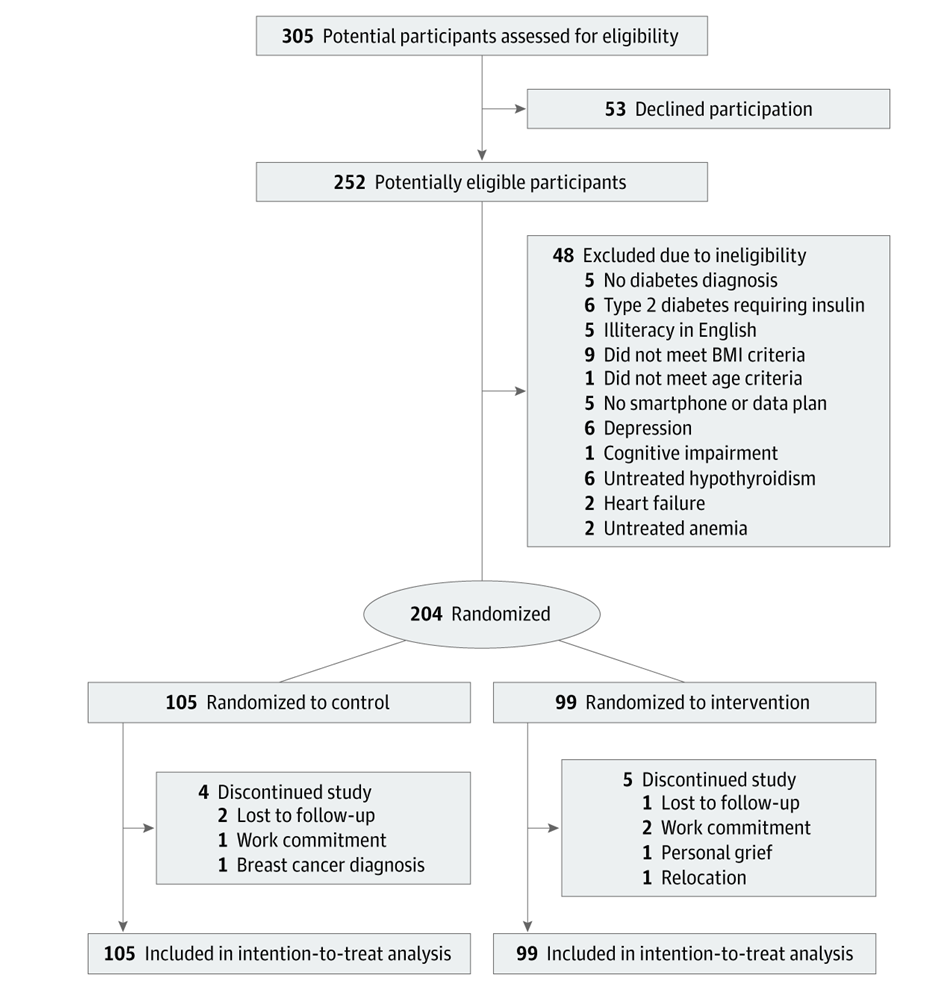
试验设计
同时,对照组和干预组的参与者均接受了营养师的饮食和身体活动建议,干预组还使用一个智能手机应用程序来跟踪其体重、饮食、体育活动和血糖,平均随访6个月。最终主要结局为体重的变化,而次要结果是血红蛋白A1c(HbA1c)、空腹血糖、血压、血脂和饮食的变化。
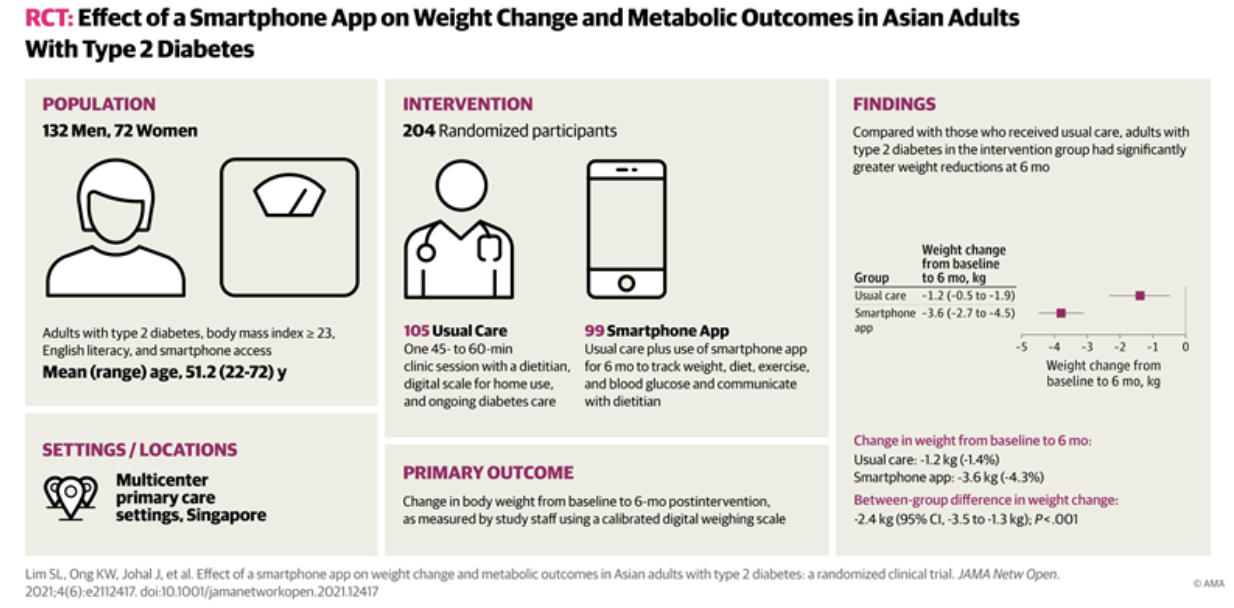
结果显示,在204名参与者中,平均年龄为51.2岁,64.7%为男性,基线平均BMI为30.6。与对照组相比,干预组体重和HbA1c水平明显下降,干预组参与者体重平均减少3.6公斤,HbA1水平平均变化为0.7%。同时,6个月时,干预组有更多的人减少了糖尿病药物治疗。
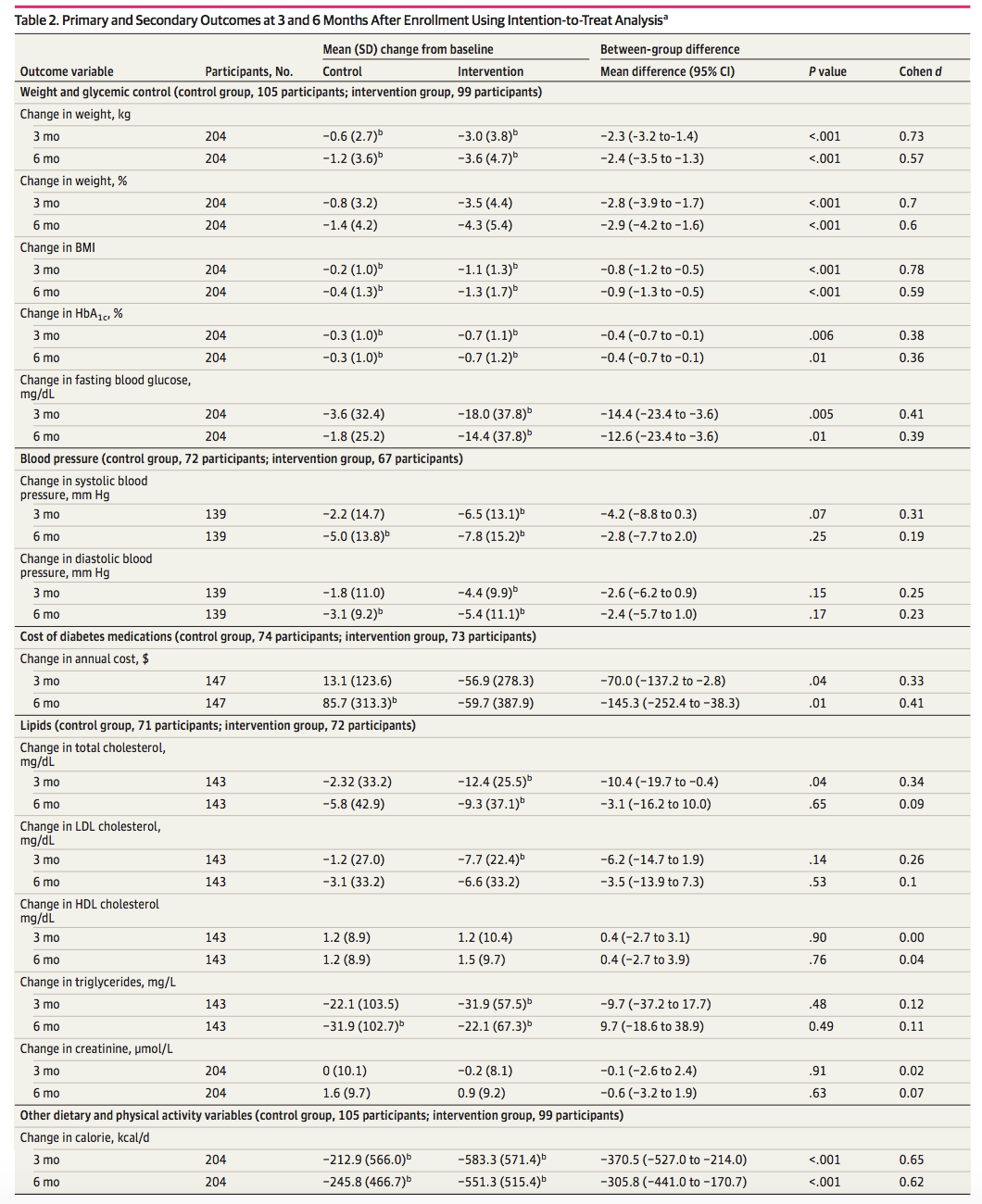
3 个月和 6 个月的主要和次要结果
在HbA1c水平为8%或更高的参与者中,干预措施使得HbA1c水平有个更大幅度的降低(平均[SD]变化,-1.8%[1.4] vs -1.0%[1.4];P = .001)。在空腹血糖、舒张压和饮食变化方面,干预组和对照组有着明显的差异。
综上,尽管减少了面对面的互动,但本研究中应用程序的使用在糖尿病患者全程管理中取得了相似的干预效果。基于智能手机的生活方式干预能够在未接受胰岛素治疗的 2 型糖尿病和超重或肥胖的亚洲成年人中实现有意义的体重减轻。此外,应用程序干预显著改善了血糖,尤其是在糖尿病控制不佳的个体中,同时减少了糖尿病药物使用。
原始出处
Su Lin Lim, PhD1; Kai Wen Ong, BSc1; Jolyn Johal, BSc2; et al.Effect of a Smartphone App on Weight Change and Metabolic Outcomes in Asian Adults With Type 2 Diabetes A Randomized Clinical Trial.JAMA Netw Open. 2021;4(6):e2112417. doi:10.1001/jamanetworkopen.2021.12417
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
34
#应用程序#
47
#PE#
33
所以科技改变生活
46
#糖尿病患者#
28
学习啦
56
学习
52
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
57
谢谢MedSci提供最新的资讯
48
写的好
36