European Radiology:增强CT和MRI在手部关节炎中的应用
2022-08-24 shaosai MedSci原创
到目前为止,双能量CT(DECT)已经发展成为诊断痛风性关节炎的重要影像学工具,CT减影(CT-S)和DECT衍生的碘图(iMap)可以检测出关节内活动性软组织炎症的造影剂摄取,并具有足够的诊断准确性
众所周知,滑膜炎和腱鞘炎的早期检测在关节炎影像学检查中具有重大意义,早期治疗可防止不可逆的骨和关节破坏,有助于保护关节功能并提高患者的生活质量。
目前的关节炎诊断标准包括肌肉骨骼超声(MSUS)和磁共振成像(MRI)。由于特异性相对较低,MRI不再是首选的成像方式。MSUS更容易获得,并提供比MRI更高的空间分辨率,已经成为诊断早期关节炎的首选影像学手段。
到目前为止,双能量CT(DECT)已经发展成为诊断痛风性关节炎的重要影像学工具,CT减影(CT-S)和DECT衍生的碘图(iMap)可以检测出关节内活动性软组织炎症的造影剂摄取,并具有足够的诊断准确性。此外,CT在检测骨侵蚀方面有决定性的优势,是一种快速、标准化的成像手段。
近日,发表在European Radiology杂志的一项研究使用iMap和CT-S这两种技术评估可疑似手部类风湿性关节炎患者的滑膜炎和腱鞘炎,并与以MSUS为参考标准的MRI比较了其诊断准确性。

本项前瞻性研究对本机构的关节炎患者进行了评估。所有患者都接受了手部的MSUS、MRI和对比度增强的DECT检查,从后者中重建了常规CT-S、基于图像的iMap(iMap-I)和基于原始数据的iMap(iMap-RD)。应用改良的类风湿性关节炎MRI评分(RAMRIS)对CT和MRI数据集的滑膜炎和腱鞘炎/副腱鞘炎进行了评分,并计算了敏感性、特异性和诊断准确性。使用单尾的McNemar检验来检验非劣效性。总分的相关性用皮尔逊检验来评估。阅读者之间的可靠性使用Cohen's kappa来评估。
总共有33名患者被纳入研究。28名患者的MSUS对滑膜炎和腱鞘炎/副腱鞘炎呈阳性,总分是6.91分。CT-S(总分6.38;r = 0.91)、iMap-RD(总分9.74;r = 0.82)、MRI(总分12.70;r = 0.85)和iMap-I(总分6.94;r = 0.50)与MSUS的相关性极佳。CT-S的诊断准确性最高,为83%,其次是iMap-I(78%)、MRI(75%)和iMap-RD(74%)。所有模式都显示出非劣质性。读者对CT-S和MRI的一致性良好(κ=0.62;0.64),对iMap-RD和iMap-I的一致性一般(κ=0.31;0.37)。
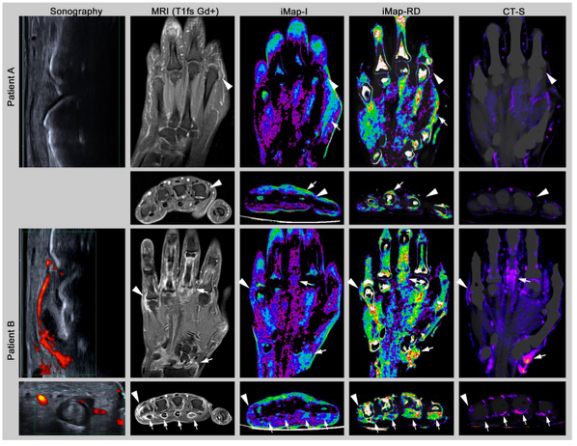
图 冠位和轴位方向的成像实例。MRI(T1fs Gd+)=脂肪饱和对比增强T1加权序列MRI;iMap-I=基于图像数据的双能量CT碘图;iMap-RD=基于原始数据的双能量CT碘图;CT-S=CT减影。患者A:50岁的女性患者,血清阴性类风湿性关节炎。未发现关节炎症变化,如掌指关节II(MCP)(箭头)。注意在骨和皮肤边界的部分容积效应(箭头)。患者B:一个55岁的女性患者,血清阴性类风湿关节炎。在MCP V(箭头)和桡骨掌关节(箭头)有严重的滑膜炎。此外,在所有的检查方式中都发现了屈肌腱II-V的严重腱鞘炎(箭头),而iMap-I往往低估了腱鞘炎III(箭头)和CT-S腱鞘炎V(箭头)
本研究表明,CT-S和iMap可以实现高度标准化的关节炎成像,并适合于临床实践。
原文出处:
Sevtap Tugce Ulas,Katharina Ziegeler,Sophia-Theresa Richter,et al.Contrast-enhanced CT techniques and MRI perform equally well in arthritis imaging of the hand: a prospective diagnostic accuracy study.DOI:10.1007/s00330-022-08744-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
38
#增强CT#
49
#关节炎#
58
签到学习
52