FASEB J:高胆固醇血症与骨关节炎的发生发展相关
2016-10-16 MedSci MedSci原创
高胆固醇不仅会损害机体的心血管系统。近期发表于FASEB的一项新的研究利用动物模型发现,高胆固醇可引发线粒体对软骨细胞的氧化应激,导致细胞死亡,并最终导致骨关节炎的发生发展。本研究测试了线粒体靶向抗氧化剂在高胆固醇诱导的骨关节炎中潜在的治疗作用,并位使用线粒体靶向抗氧化剂治疗骨关节炎提供证据支持。研究人员使用两种不同的动物模型来模拟人类高胆固醇血症。第一种动物模型是携带改变基因的小鼠,这个基因称为
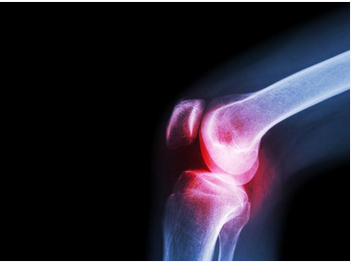
高胆固醇不仅会损害机体的心血管系统。近期发表于FASEB的一项新的研究利用动物模型发现,高胆固醇可引发线粒体对软骨细胞的氧化应激,导致细胞死亡,并最终导致骨关节炎的发生发展。
研究人员使用两种不同的动物模型来模拟人类高胆固醇血症。第一种动物模型是携带改变基因的小鼠,这个基因称为ApoE-/ ,此基因可使动物发生高胆固醇血症。另一个大鼠模型饲以高胆固醇饮食,导致饮食诱导的高胆固醇血症。对两组鼠进行手术以模仿人膝盖受伤,然后对两组鼠饲以胆固醇饮食或正常饮食。
结果发现,无论是小鼠和大鼠,进行手术和饲以高胆固醇饮食组出现骨性关节炎严重程度较正常饮食组高。然而,与未处理组相比,当两组小鼠和大鼠接受降胆固醇药物阿托伐他汀和线粒体靶向抗氧化剂治疗后骨关节炎的发生显著降低。
总而言之,该研究发现,与骨关节炎的发生发展相关的另一个研究点——高胆固醇血症。
原始出处:
High cholesterol triggers mitochondrial oxidative stress leading to osteoarthritis. Science Daily, October 14, 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生发展#
36
#骨关节#
29
#FAS#
38
#关节炎#
27
#高胆固醇血症#
38
学习新液,谢谢。
66