Sci Transl Med:环糊精有望治疗动脉粥样硬化
2016-04-15 新华社 郭洋 《科学转化医学》
德国等国研究人员6日在美国《科学转化医学》杂志上报告说,环状低聚糖——环糊精可起到阻止甚至减少胆固醇结晶沉积的作用,有望用于治疗动脉粥样硬化。 动脉粥样硬化是指动脉壁上沉积一层包括胆固醇结晶在内的粥样物质,使动脉弹性降低、管腔变窄,常导致心肌梗塞、中风等致命疾病发生。胆固醇结晶会引发免疫反应,导致动脉壁出现可致命的炎症。 先前研究发现,环糊精可缓解先天性糖脂代谢性疾病——C型尼曼匹克氏症患者脑
德国等国研究人员6日在美国《科学转化医学》杂志上报告说,环状低聚糖——环糊精可起到阻止甚至减少胆固醇结晶沉积的作用,有望用于治疗动脉粥样硬化。
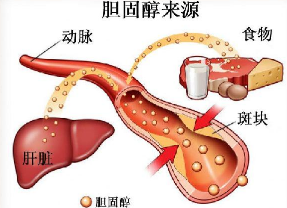
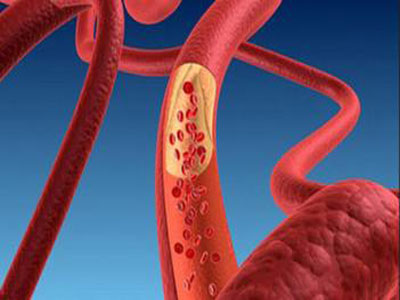
动脉粥样硬化是指动脉壁上沉积一层包括胆固醇结晶在内的粥样物质,使动脉弹性降低、管腔变窄,常导致心肌梗塞、中风等致命疾病发生。胆固醇结晶会引发免疫反应,导致动脉壁出现可致命的炎症。
先前研究发现,环糊精可缓解先天性糖脂代谢性疾病——C型尼曼匹克氏症患者脑细胞内的胆固醇运输障碍。德国波恩大学等机构的研究人员据此猜测,环糊精可能有助于清除动脉粥样硬化患者动脉壁上沉积的胆固醇结晶
研究人员持续8周给实验鼠喂食高胆固醇食物,并给一部分实验鼠注射了环糊精。结果显示,实验鼠在注射环糊精后,血管中的沉积物要比其他实验鼠少很多。环糊精提高了细胞清除胆固醇的能力,并减少了血管中的炎症反应。研究人员利用人类动脉粥样硬化患者血管中的沉积物展开的研究也得出上述结论。
研究人员表示,环糊精可用于研发动脉粥样硬化治疗药物。不过,虽然环糊精作为一些难溶性药物的增溶剂早已进入市场,但将其作为治疗动脉粥样硬化的新药还需进一步临床研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
37
#Transl#
46
#粥样硬化#
30
#Med#
28
这就是创新
100
中医药
119
记住环瑚精
152
高大上的文章
120
值得关注
123