CLIN CANCER RES:血管靶向光动力疗法可以增强PD-1/PD-L1通路阻滞抗肿瘤免疫反应
2018-02-25 MedSci MedSci原创
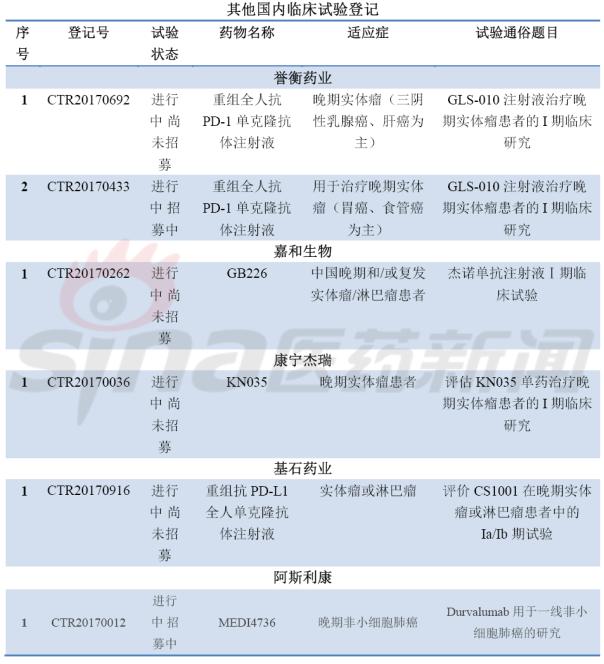
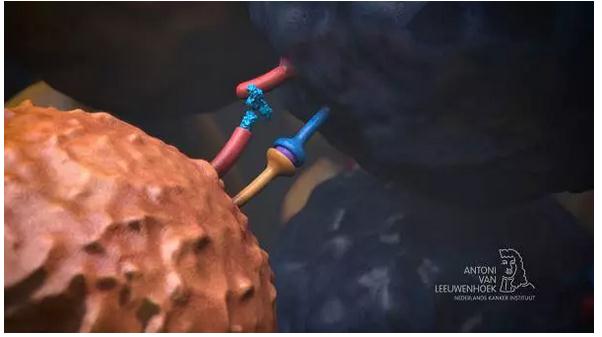
PD-1/PD-L1通路抑制可以有效治疗晚期肾细胞癌。但是其结果变化很大,可能取决于宿主因素,包括肿瘤微环境。使用光敏剂WST11的血管靶向光动力疗法(VTP)可以诱导局部免疫反应。CLIN CANCER RES近期发表了一篇文章,研究光动力疗法是否可以增强PD-1通路抑制的局部和系统抗肿瘤反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PD-L1#
41
#免疫反应#
39
#光动力#
33
谢谢分享学习
0
非常好的文章.学习了
72
好
74