JACC:半乳凝素3的变化可预测心血管疾病风险
2018-12-23 MedSci MedSci原创
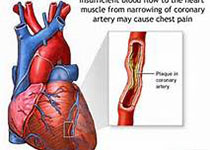
半乳凝素3(Gal-3)与心衰和不良心血管预后相关,然而,Gal-3的纵向变化对临床结果的影响尚不清楚。本研究的目的旨在评估影响社区居住人群Gal-3变化的临床因素,以及Gal-3的变化与心衰、心血管疾病和死亡率的相关性。本研究对2477名弗雷明翰心脏研究后代队列中的对象进行了两次血浆Gal-3的测量(1995-1998和2005-2008),并通过线性回归模型评估影响Gal-3变化的因素。研究结
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
35
学习学习天天向上
83
#ACC#
28
#疾病风险#
39
#血管疾病#
0
好
87