BMC Cancer:局部晚期非小细胞肺癌(LA-NSCLC)放化疗后durvalumab治疗可改善患者的预后
2022-04-08 yd2015 网络
研究表明,局部晚期非小细胞肺癌(LA-NSCLC)放化疗后durvalumab治疗可改善患者的预后。
近期,BMC Cancer杂志上发表了一项真实世界研究成果,主要是评估局部晚期非小细胞肺癌(LA-NSCLC)放化疗后durvalumab治疗对患者预后的影响。
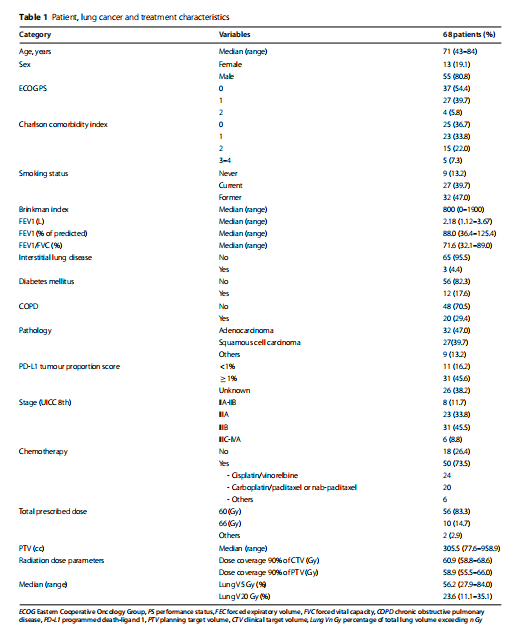
研究纳入68例患者,无一例患者接受诱导化疗,50例(73.5%)患者接受同时放化疗。36名患者接受了durvalumab治疗。
中位随访14.3个月,23例患者死亡,37例患者发生肿瘤进展,其中28例患者发生远处转移。1年DMFS率、PFS率和OS率分别为59.9%(95%可信区间[CI]: 46.8 70.7%)、48.7%(95% CI: 35.8 60.3%)和84.2% (95% CI: 72.5 91.2%)。根据是否使用durvalumab治疗,可以发现durvalumab的治疗改善患者的OS、DMFS和PFS。
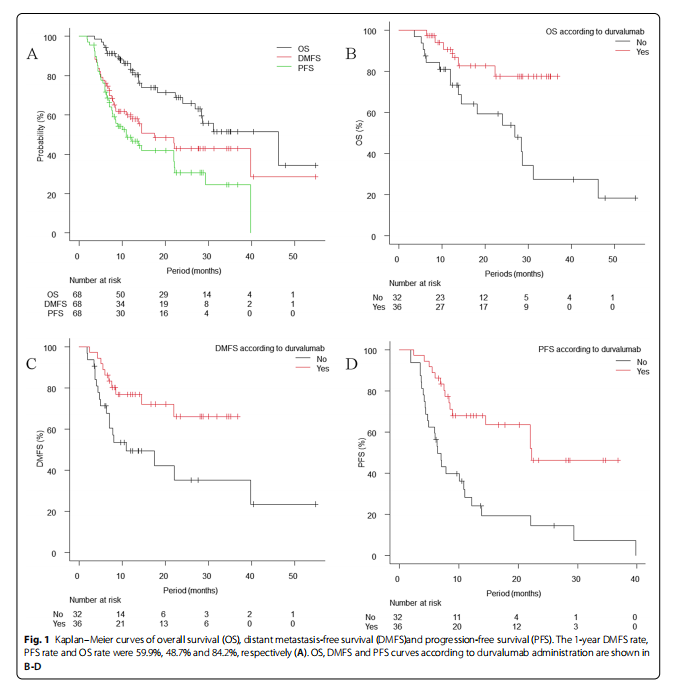
多因素分析结果显示,durvalumab的应用使得DMFS、PFS和OS的危险比(HR)显著降低(HR 0.31, 95% CI 0.14–0.69, p<0.01, HR 0.33, 95% CI 0.15–0.69, p<0.01 and HR 0.32, 95% CI 0.12–0.86, p=0.02)。

IIIA期和IIIB-IIIC期DMFS、PFS和OS的比较,差异均无统计学意义(HR = 1.08, p=0.83, HR = 0.97, p=0.93, HR = 1.11, p=0.82)。在使用durvalumab的患者中,PD-L1 ≧1%和PD-L1<1%患者在DMFS、PFS和OS中差异不显著(HR 0.44, p=0.35, HR 0.66, p=0.61和HR 0.46, p=0.51)。
综上,研究表明,局部晚期非小细胞肺癌(LA-NSCLC)放化疗后durvalumab治疗可改善患者的预后。
原始出处:
Yamamoto T, Tsukita Y, Katagiri Y, Matsushita H, Umezawa R, Ishikawa Y, Takahashi N, Suzuki Y, Takeda K, Miyauchi E, Saito R, Katsuta Y, Kadoya N, Jingu K. Durvalumab after chemoradiotherapy for locally advanced non-small cell lung cancer prolonged distant metastasis-free survival, progression-free survival and overall survival in clinical practice. BMC Cancer. 2022 Apr 4;22(1):364. doi: 10.1186/s12885-022-09354-1. PMID: 35379201.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#局部晚期#
39
#mAb#
27
#非小细胞#
33
#BMC#
35
#放化疗#
39
#局部#
23
学习了,谢谢分享
33