ACS Biomaterials:浙大贺永教授成功进行跨尺度血管结构的生物3D打印
2017-02-19 贺永 贺永博客
心血管疾病是当今世界威胁人类最严重的疾病之一,其作用机制复杂,目前基于动物实验及平面细胞实验的研究与人体环境相差甚远,如果能够在体外构建一个可以模拟体内血管环境的血管模型,在这个模型上进行化学刺激和力学刺激,将会为心血管疾病机理的探讨提供高效的工具。我们团队经过两年多的研究探索,提出了一种血管3D打印工艺,该工艺能实现宏微跨尺度血管结构的打印,宏观流道可用于各种机械力的加载,微观通道可用于营养输送
心血管疾病是当今世界威胁人类最严重的疾病之一,其作用机制复杂,目前基于动物实验及平面细胞实验的研究与人体环境相差甚远,如果能够在体外构建一个可以模拟体内血管环境的血管模型,在这个模型上进行化学刺激和力学刺激,将会为心血管疾病机理的探讨提供高效的工具。我们团队(注:浙江大学贺永教授团队)经过两年多的研究探索,提出了一种血管3D打印工艺,该工艺能实现宏微跨尺度血管结构的打印,宏观流道可用于各种机械力的加载,微观通道可用于营养输送以及化学物质的加载。本血管打印模型可以集成在器官芯片上,可应用于药物筛选、细胞共培养、细胞力学等领域,本研究受到国家基金重点项目、国家优秀青年基金、浙江省杰出青年基金项目资助。
基于生物打印的方法在体外构建血管结构一直是组织工程领域的研究热点,常见的方法主要包括:直接打印管状结构和在凝胶结构中构建流道网络,虽然这些方法制造出的血管模型在一定程度上可以模拟真实血管的功能,但是它们无法同时满足化学加载和力学加载的要求,故无法用于体外模拟血管环境平台的搭建,进而难以用于血管类疾病机理的研究。
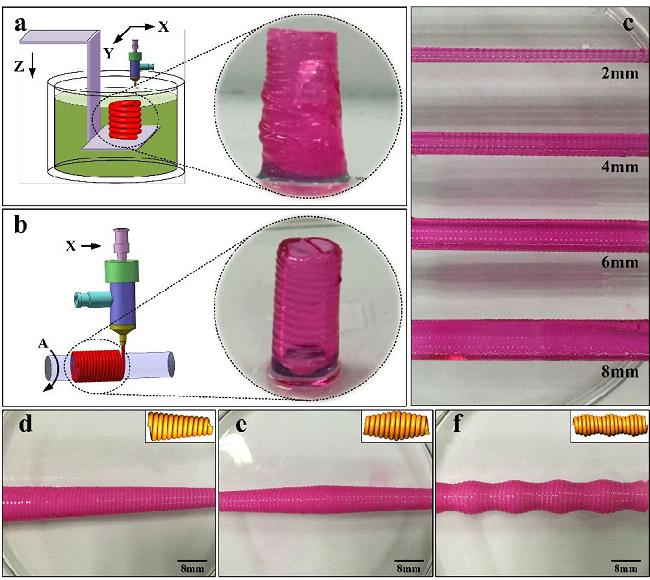
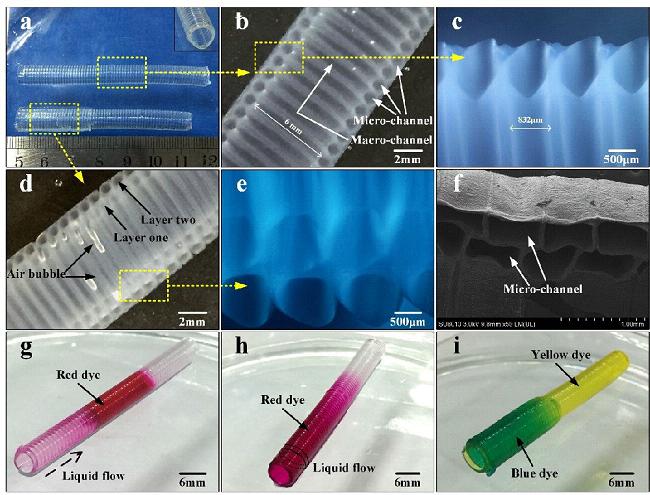
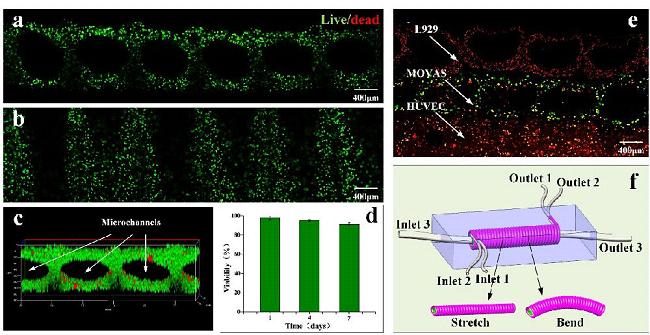
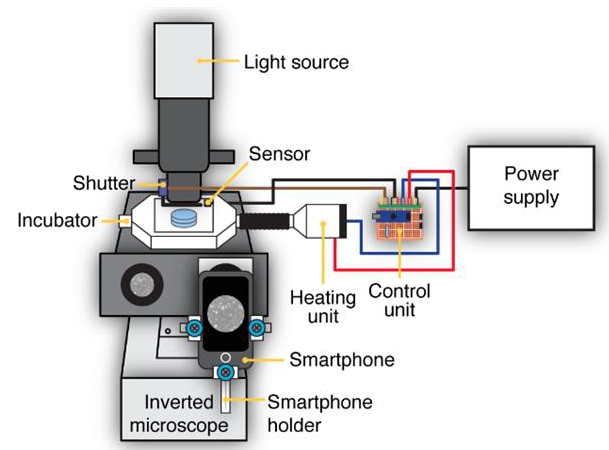
我们提出了一种全新的血管打印方法,其特点是能实现宏微跨尺度流道的同时成形。通过课题组自行研发的血管打印机,利用同轴喷头制造出中空凝胶纤维,装载成纤维细胞和平滑肌细胞的凝胶纤维可控沉积在三维打印平台中的旋转模板上,内皮细胞种在中空凝胶纤维融合后形成的宏观通道内。课题组通过大量的工艺实验,系统解决了跨尺度血管结构的成型问题;通过流体流动实验演示了多尺度流道的用处;并通过后续的三层细胞培养实验展示了在组织工程应用中的可能性。
我们很欣慰的是通过这个研究,将生物3D打印机实现了产业化,预计今年6月份将能批量提供,本生物3D打印机及生物制造套件可实现包括可打印血管等含细胞的生物组织、人工骨等陶瓷材料、载药支架等的高效制造。欢迎感兴趣的老师联系我,继续就这一领域进行深化研究哈,yongqin@zju.edu.cn
题外话:ACS Biomaterials延续了ACS出版社的一贯高质量要求,共4个审稿人意见都非常专业,我们的Response Letter就足足写了30页。


原始出处:
Qing Gao,et al. 3D Bioprinting of Vessel-likeStructures with Multilevel Fluidic Channels.DOI:10.1021/acsbiomaterials.6b00643
原文下载:3D Bioprinting of Vessel-like Structures with Multilevel Fluidic Channels.pdf
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
31
#血管结构#
46
#Biomaterials#
44
作用机制复杂
74
#ACS#
36
#3D#
32
#浙大#
31
3D打印技术
58
好好努力
64
最终幻想终成现实
57