幼儿胼胝体区动静脉瘘伴巨大静脉瘤1例
2020-01-09 李强 张昌伟 林森 四川医学
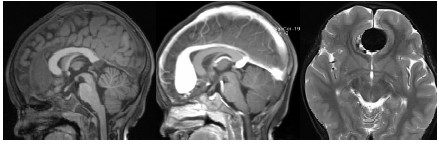
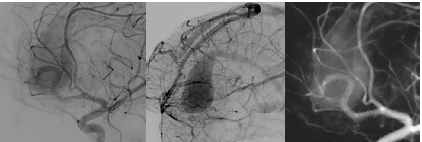
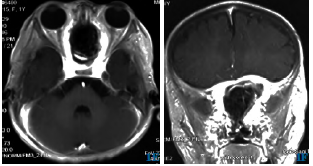
患者,女,3岁9月,因“检查发现额部血管畸形3d”入院。患者入院前3d因发热伴抽搐于当地医院就诊,查颅脑MRI发现胼胝体膝部占位,伴流空效应,见图1。患者无头痛、头晕、恶心、呕吐等症状。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章
0
#静脉#
30
#静脉瘤#
41
#胼胝体区#
0
#胼胝体#
33
#动静脉瘘#
55