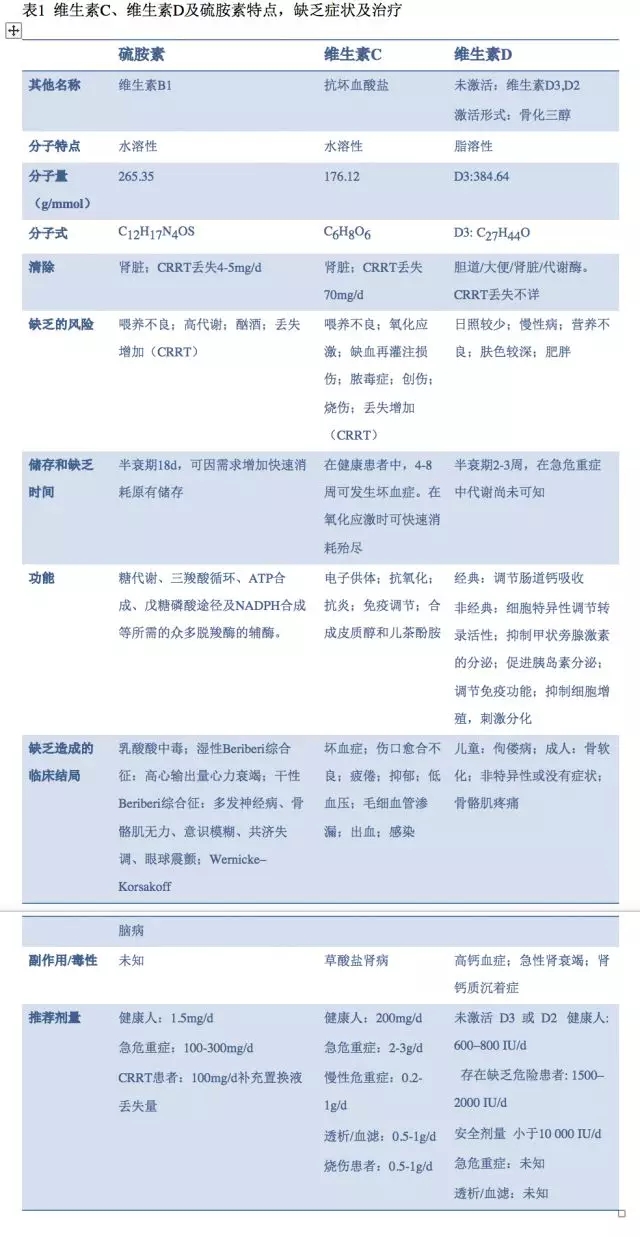
Intensive Care:重症患者的维生素治疗:关注维生素B1,维生素C及维生素D
2018-04-14 胡婕 周飞虎 重症医学
译者:自从2017年Paul E. Marik 教授在chest发表脓毒症代谢复苏的研究后(Chest 2017, 151(6):1229-1238),代谢复苏就成为脓毒症治疗的一个较为热门且极富争议性的话题。因此,我们把ICM最新发表的一篇综述翻译呈献给国内的重症人,希望给大家在脓毒症治疗上带来新的思路!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TENS#
23
学习了
51
#重症患者#
22
#维生素B#
21
好好文献.学习了
51
学习了.长知识
58
阅
54