颈内静脉穿刺不顺?注意颈内静脉瓣!
2014-07-17 张华斌 新青年麻醉论坛
注意颈内静脉瓣 静脉瓣是静脉壁上防止静脉反流的瓣膜结构,主要见于肢体静脉系统。内脏静脉、头部静脉内和头臂静脉内没有静脉瓣,但在颈内静脉内有一对静脉瓣,是心脏与脑之间唯一的一对静脉瓣。颈内静脉瓣防止心房收缩时的颈内静脉反流,从而维持颅内静脉压的稳定和平衡,是重要的解剖结构。 但很多超声医师对这一结构不熟悉,常常把它误认为异常结构,甚至有把其当作颈静脉内膜剥离作为病例报道的笑话
注意颈内静脉瓣
静脉瓣是静脉壁上防止静脉反流的瓣膜结构,主要见于肢体静脉系统。内脏静脉、头部静脉内和头臂静脉内没有静脉瓣,但在颈内静脉内有一对静脉瓣,是心脏与脑之间唯一的一对静脉瓣。颈内静脉瓣防止心房收缩时的颈内静脉反流,从而维持颅内静脉压的稳定和平衡,是重要的解剖结构。
但很多超声医师对这一结构不熟悉,常常把它误认为异常结构,甚至有把其当作颈静脉内膜剥离作为病例报道的笑话,因此有必要对这一解剖结构做一介绍。
颈内静脉瓣位于颈内静脉根部,大致位于锁骨水平,个体之间位置略有差异,左侧位置较低。颈静脉瓣由前后两个瓣叶构成,随着心动周期的变化,可以见到瓣叶规律性的开合。声像图上颈静脉瓣呈带样强回声,根部附着于静脉壁上,瓣膜游离缘指向心脏方向,实时检查时可见瓣膜的关闭过程。利用M型超声可以清晰地显示瓣叶的运动规律和开闭。(图1,,2,3)

图1 正常颈内静脉瓣(前瓣叶未显示)

图2 颈内静脉的开合过程

图3 颈内静脉瓣的M型成像,显示瓣叶的规律性开合
颈内静脉瓣的临床意义
颈内静脉瓣作为心脏于脑之间的唯一的瓣膜结构,起着防止静脉反流维持颅内静脉压稳定的重要作用。
临床实践中,颈内静脉穿刺置管是急重症医学和麻醉科非常重要的操作,偶尔有穿刺后导丝不能顺利下行的状况出现,这就是因为导丝顺管壁下行过程中遇静脉瓣根部阻挡所致(图4)。本人曾经遇过两例,在超声引导下通过调整导丝位置得以置管成功。

图4 颈内静脉置管是导丝受静脉瓣根部阻挡,长白箭:血流方向,绿箭:导丝
颈内静脉瓣膜功能不全导致颈内静脉反流(图5),特别是在患者做Valsava样动作(如咳嗽、排便等)时,就会造成颅内静脉压一过性的增高。有几个研究显示颅内静脉压的升高与偏头痛的进展相关。
Chuang 等则报告了颈内静脉或椎静脉反流与良性咳嗽性头痛有关。
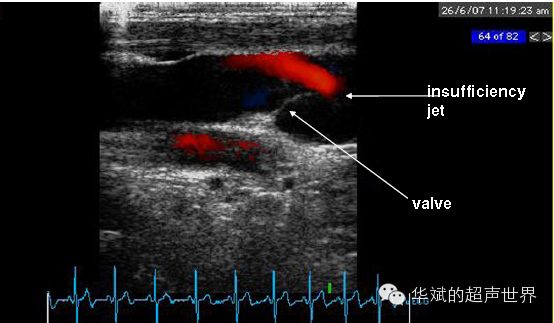
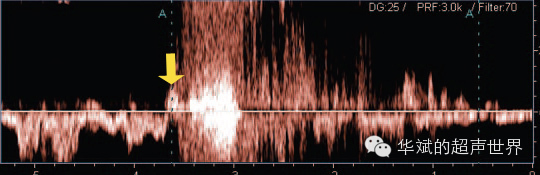
图5 颈静脉瓣功能不全。上图红色血流为瓣膜关闭不全形成的反流信号,下图为频谱多普勒显示的反流信号。黄箭:Valsava动作。
(作者:张华斌 华斌的超声世界)
(作者:张华斌 华斌的超声世界)
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








我第一次超声下遇到颈内V瓣时也有点疑惑,但仔细一看无论形态和功能都象Ⅴ瓣,欧了。
35
值得收藏,学习,谢谢分享
102
#静脉#
42
#颈内静脉#
35
#穿刺#
37
#静脉穿刺#
31