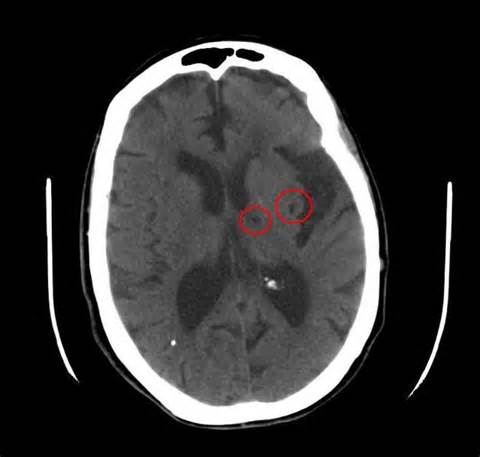
Stroke: IL-6和TNF受体预测腔隙性脑梗死后卒中再发
2016-05-24 MedSci MedSci原创
背景:研究者假设:白细胞介素6(IL-6)浓度,血清淀粉样蛋白A、肿瘤坏死因子-α受体1,CD40配体,和单核细胞趋化蛋白1能够预测近期腔隙性脑梗死后卒中再发和主要血管事件的发生。方法:卒中治疗的炎症标志物水平(LIMITS)是一个国际多中心前瞻性的配套的生物标志物研究,嵌套在皮层下卒中二级预防研究(SPS3),是一项近期腔隙性脑梗的III期临床试验。应用Cox比例风险模型和校正模型计算卒中再发风
背景:研究者假设:白细胞介素6(IL-6)浓度,血清淀粉样蛋白A、肿瘤坏死因子-α受体1,CD40配体,和单核细胞趋化蛋白1能够预测近期腔隙性脑梗死后卒中再发和主要血管事件的发生。
方法:卒中治疗的炎症标志物水平(LIMITS)是一个国际多中心前瞻性的配套的生物标志物研究,嵌套在皮层下卒中二级预防研究(SPS3),是一项近期腔隙性脑梗的III期临床试验。应用Cox比例风险模型和校正模型计算卒中再发风险的HR值和95% CI。
结果:1244例腔隙性卒中(平均年龄63.3±10.8年),115个主要的血管事件(卒中、心肌梗死、血管性死亡)发生。主要血管事件风险随肿瘤坏死因子-α受体1(每SD校正HR,1.21;95% CI,1.05-1.41;P = 0.01)和白细胞介素-6(每SD校正HR,1.10;95% CI,1.02-1.19;P = 0.008)增加而增加。校正人口学资料后,与最低四分位数相比(肿瘤坏死因子-α受体1<2.24ng/L),最高四分位数(肿瘤坏死因子-α受体1>3.63 ng/L)的患者主要血管事件发生的风险增加两倍(部分校正HR,1.98;95% CI,1.11-3.52),在校正其他危险因素和他汀类药物使用后这种效应稍有减弱(校正HR,1.68;95% CI,0.93-3.04)。血清淀粉样蛋白A,CD40配体,和单核细胞趋化蛋白1与预后无相关性。
结论:腔隙性脑梗死患者中,IL-6和TNF受体浓度预测血管事件复发的风险,并且与抗血小板治疗效果相关。
原始出处:
Boehme AK, McClure LA, et al. Inflammatory Markers and Outcomes After Lacunar Stroke: Levels of Inflammatory Markers in Treatment of Stroke Study. Stroke. 2016 Mar
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TNF受体#
18
#IL-6#
30
#TNF#
29
#脑梗#
30