Stroke:房颤并发心力衰竭患者左心功能不全程度、症状与栓塞风险之间关系
2015-02-02 李志行 译 MedSci原创
目前在房颤患者中左心室功能障碍(LVSD)、心力衰竭(HF)症状、栓塞风险之间关系方面的数据十分有限。研究方法:HF患者参与氯吡格雷联合厄贝沙坦预防房颤患者血管事件(ACTIVE)试验,但并不随机分配口服抗凝药物,他们被归类为保存射血分数型心衰和减低射血分数型心衰。如果是减低型,LVSD被分为轻度、中度或重度。症状通过纽约心脏病协会分级进行定量。主要结果为中风、短暂性脑缺血发作和全身性栓塞的综合。
目前在房颤患者中左心室功能障碍(LVSD)、心力衰竭(HF)症状、栓塞风险之间关系方面的数据十分有限。
研究方法:
HF患者参与氯吡格雷联合厄贝沙坦预防房颤患者血管事件(ACTIVE)试验,但并不随机分配口服抗凝药物,他们被归类为保存射血分数型心衰和减低射血分数型心衰。如果是减低型,LVSD被分为轻度、中度或重度。症状通过纽约心脏病协会分级进行定量。主要结果为中风、短暂性脑缺血发作和全身性栓塞的综合。
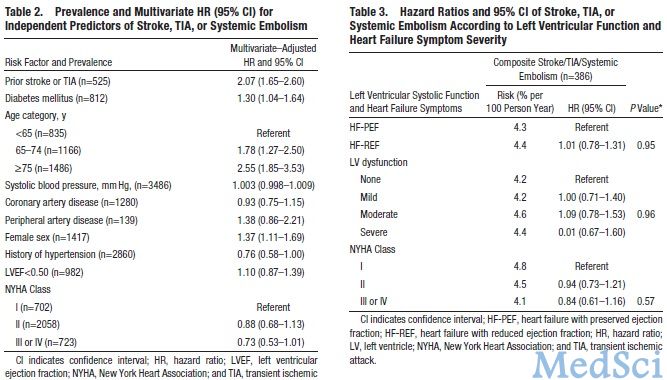
以3487名接受抗血小板治疗的HF患者做为基线。在这些患者中,有969名(46.8%)保存射血分数型HF患者和1103名 (53.2%)减低射血分数型HF患者。在3.6年的平均随访期内,386名患者首次发生中风、短暂性脑缺血发作或全身性栓塞。栓塞最强的独立预测指标为年龄 ≥75 岁(HR 2.55; CI, 1.85–3.53),中风或短暂性脑缺血发作先兆(HR 2.07; 95% CI, 1.65–2.60),和女性(HR 1.37; CI, 1.11–1.69)。然而,射血分数<0.50,LVSD程度和纽约心脏病协会分级并没有预测栓塞的发生。保存射血分数型HF患者与减低射血分数型HF患者表现出的发生栓塞的风险是相似的:每100人年中4.3% 对4.4%(HR 1.01; 95% CI, 0.78–1.31)。在LVSD分类(P for trend =0.96)和纽约心脏病协会分级(P for trend =0.57)中,发生栓塞的风险是相似的。
在ACTIVE试验中的HF患者中,无论是患有LVSD还是症状严重程度都不能影响发生栓塞的风险。
Roopinder K. Sandhu, Stefan H. Hohnloser, Marc A. Pfeffer, Fei Yuan, Robert G. Hart, Salim Yusuf, Stuart J. Connolly, Finlay A. McAlister, and Jeff S. Healey
Relationship Between Degree of Left Ventricular Dysfunction, Symptom Status, and Risk of Embolic Events in Patients With Atrial Fibrillation and Heart Failure
Stroke 2015; first published on January 27 2015 as doi:10.1161/STROKEAHA.114.007140
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#并发#
26
已阅
107
明白
63
#心功能不全#
44
#心功能#
31