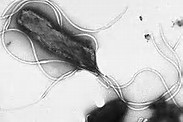
Helicobacter:日本幽门螺杆菌根除治疗对胃癌的影响
2017-12-10 杨佳佳 叶峰 消化客
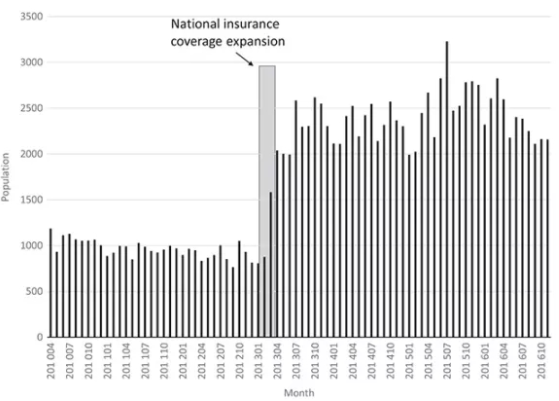
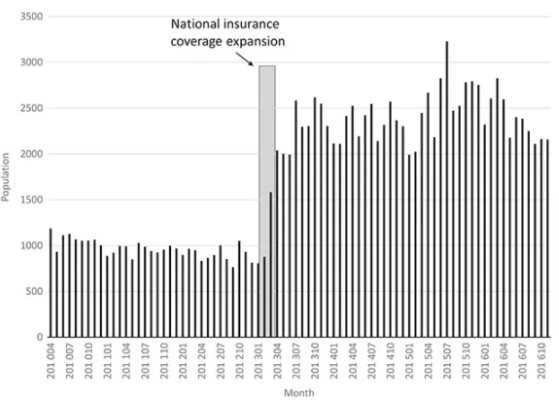
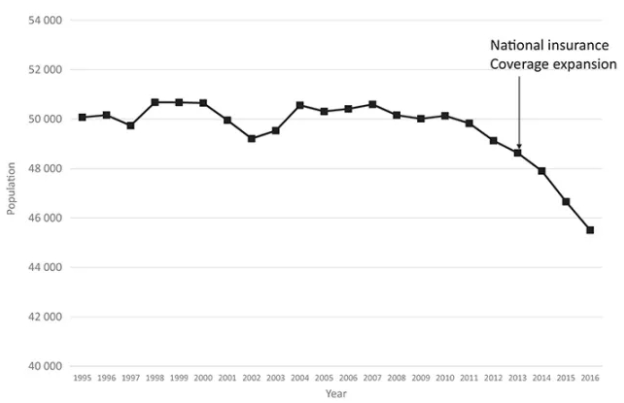
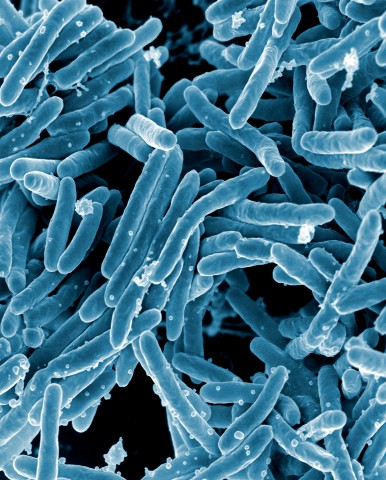
在日本,每年大约50000人死于胃癌,持续超过40年且无太大变化。据报道,日本大多数胃癌是由幽门螺杆菌(Hp)感染引起的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#螺杆菌#
29
#根除#
23
#幽门螺杆菌根除治疗#
28
#Helicobacter#
40
#根除治疗#
32
非常好.学习了
46
一起学习一下
57
#日本#
25
不错,学习了。
72
学习学习.继续关注
55