J Gastroenterol:炎症性肠病的全新治疗方案
2018-09-01 消化客 江苏省人民医院消化科
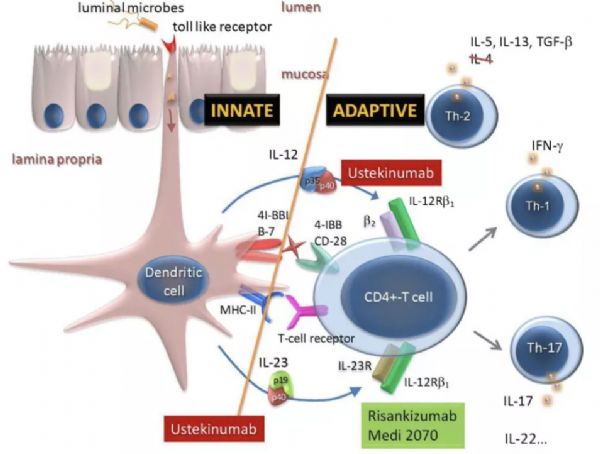
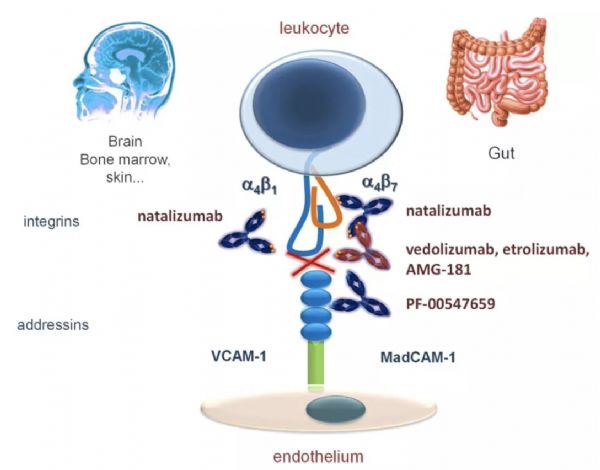
在过去的15年中,抗肿瘤坏死因子(TNF)药物的出现极大地改变了IBD的治疗策略,但其存在的最主要的问题是频发的继发性药物反应丧失。所幸的是目前探索出来的新的治疗方案,部分已经进入临床实践中。在抗细胞因子制剂中,抗-IL12/IL23单克隆抗体(mAb)已经在克罗恩病(CD)中用抗p40单克隆抗体-ustekinumab,进入临床实践。此外,更具选择性的抗IL23药物(抗p19)已经显示出疗效
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
40
#治疗方案#
38
#Gastroenterol#
40
#AST#
38
#炎症性#
54
学习了谢谢
0
期待早日用于临床
74
炎症性肠病的治疗。
1
学习学习学习
72
学习了感谢分享
80