BMJ:你发现这张普通膝关节平片中暗藏的典型标志了吗?-案例报道
2016-11-24 haofan MedSci原创
膝部外伤患者,尤其是当病人描述出现外旋外翻运动时,在膝关节侧位片上应注意寻找股骨外侧切迹征。股骨外侧切迹征往往提示膝关节前外侧旋转不稳定以及需要进行MRI检查来评估软组织损伤程度。
一名健康的23岁足球运动员在左膝盖创伤后几个小时入院。跑步的时候,患者不得不通过转动右脚来保持左脚不动(外旋外翻应力)。患者没有听到也没感觉到爆裂声或咔嚓声,但随后左脚无法承重,并直接出现肿胀和内侧局部疼痛。X线结果如下(图1)。

图1 左膝侧位片
问题:X片上有什么异常表现,这种表现可能与哪种疾病有关?
答案:股骨外侧切迹或沟征(红线)所示,这是提示存在前交叉韧带断裂(图2)。
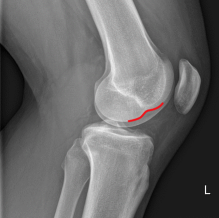
图2 左膝侧位片出现股骨外侧髁凹陷(红线)。
讨论
侧位平片显示股骨外侧切迹出现过深的异常凹陷(图2)。这种典型的中外侧股骨髁软骨凹陷是因胫骨平台后外侧受到外部强力所致。在文献中对(前交叉韧带断裂)引起的凹陷深度有两种定义,Cobby等人使用
学习点
膝部外伤患者,尤其是当患者描述出现外旋外翻运动时,在膝关节侧位片上应注意寻找股骨外侧切迹征。股骨外侧切迹征往往提示膝关节前外侧旋转不稳定以及需要进行MRI检查来评估软组织损伤程度。
原始出处:
Paul T P W Burgers, et al. A typical sign on a plain knee radiograph. BMJ.23 November 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#BMJ#
26
文章不错,值得学习
64
x片协助诊断,MRI才是硬道理
73
嗯,很有用!
64