合并多支血管病变高危心梗患者:抗血小板治疗也需更强、更长
2018-05-03 佚名 医学界心血管频道
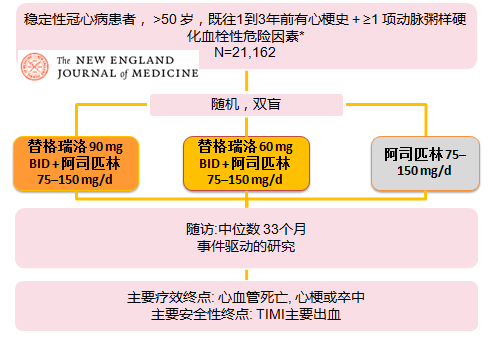
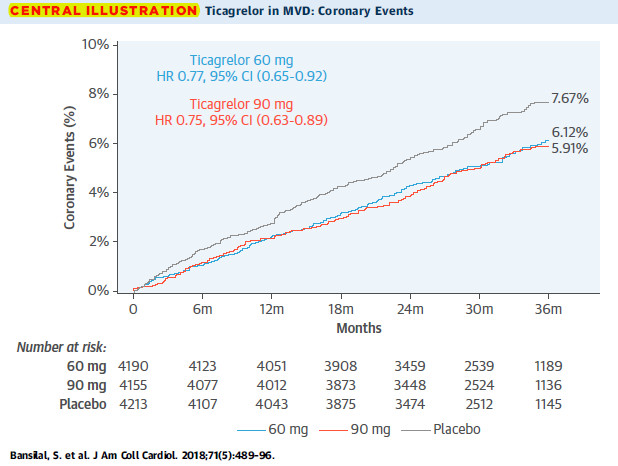
最近发表于《美国心脏病学会杂志(JACC)》的PEGASUS-TIMI 54研究亚组分析结果发现,在合并多支血管病变高危心梗患者,选用强效抗血小板药物P2Y12受体拮抗剂,并延长双抗的疗程(中位随访时间33个月),可显着降低冠脉事件,且不增加致死性出血及颅内出血风险。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心梗患者#
41
#血管病#
29
#多支血管#
38
#血管病变#
26
学习.谢谢分享
81
学习了
83
学习学习
81
学习谢谢分享
76
谢谢分享.学习了
71
谢谢分享学习了
26