Cardiovasc Diabetol:IL-12/23p40水平升高可作为2型糖尿病心率变异性功能障碍的潜在指标
2022-01-15 MedSci原创 MedSci原创
心脏功能和血清标志物特别是IL-12/IL-23p40之间有很强的相关性,提示促炎因子、内皮细胞和淋巴功能的系统性改变会影响整体心血管功能。
心血管疾病(CVD)是2型糖尿病(T2D)发病和死亡的主要原因,约占所有死亡的50%。心血管功能包括心率、心脏收缩性和血压是由自主交感神经迷走神经平衡调节的,在糖尿病患者中,这一平衡可能因糖尿病神经病变而发生倾斜。
全身炎症过程似乎有助于心血管并发症的发展,导致2型糖尿病发病率和死亡率的增加。循环炎症标志物,即白介素(IL)-6和肿瘤坏死因子-α,与神经心脏测量相关。研究者对各种炎症和炎症相关的血清标志物进行了广泛的研究,以了解心血管调节和全身炎症水平之间可能的神经免疫相互作用。
研究人员分析了100名2型糖尿病患者的血清样本。根据心电图读数进行心率变异性、心血管自主反射试验和心脏迷走神经张力试验。记录了相关数据(人口统计学、糖尿病和心血管危险因素)。
结果显示,血清IL-12/IL-23p40(p<0.01)和细胞间粘附分子(ICAM)-1(p<0.007)水平升高与心率变异性测量值降低相关。在所有调整后,IL-12/23p40、SDANN和VLF之间的相关性持续存在(p=0.001)。此外,血清血管内皮生长因子(VEGF)-C水平与站立反应相关(p=0.005)。
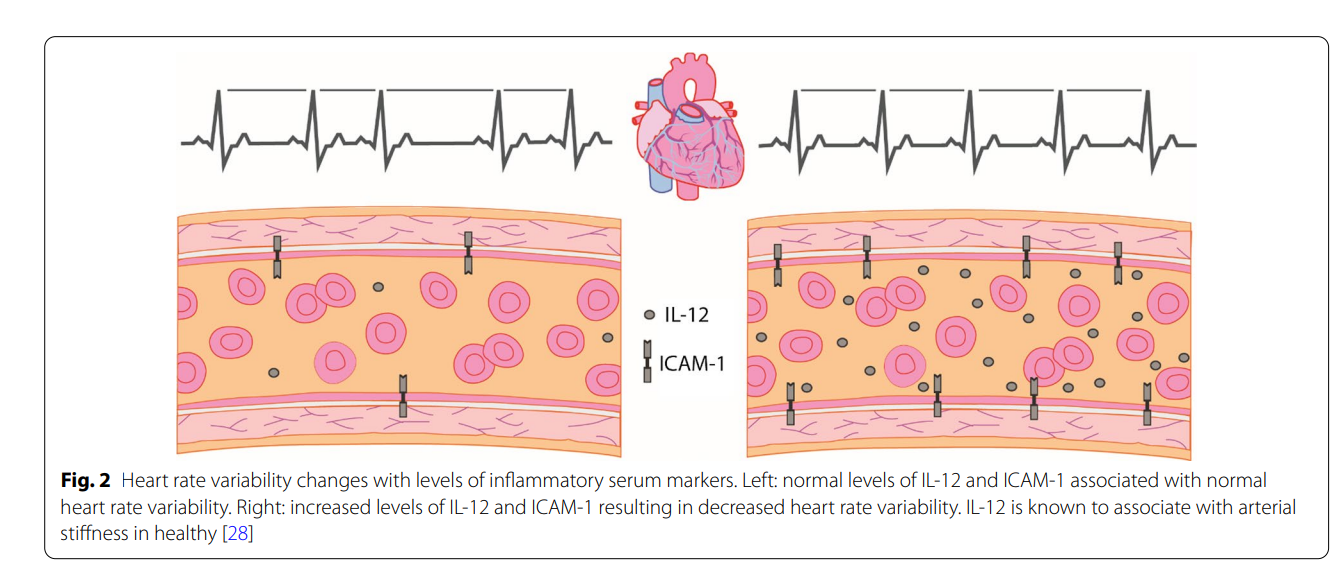
心率变异性随炎症血清标志物水平而改变。左:正常水平的IL-12和ICAM-1与正常心率变异性相关。右图:IL-12和ICAM-1水平升高导致心率变异性降低。IL-12已知与健康的动脉硬化有关。
总之,本研究发现心脏功能和血清标志物特别是IL-12/IL-23p40之间有很强的相关性,提示促炎因子、内皮细胞和淋巴功能的系统性改变会影响整体心血管功能。尽管该研究采用了横断面设计,但强有力的结果不受协变量的影响。进一步了解它们潜在的心血管机制可能会发现新的药物干预靶点,未来可期。
参考文献:Wegeberg, A.M., Okdahl, T., Riahi, S. et al. Elevated levels of interleukin-12/23p40 may serve as a potential indicator of dysfunctional heart rate variability in type 2 diabetes. Cardiovasc Diabetol 21, 5 (2022). https://doi.org/10.1186/s12933-021-01437-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#IL-12#
40
#BET#
32
#ASC#
24
#DIA#
26
#变异#
29
#功能障碍#
31
#心率变异性#
43
#IL-1#
30