Science Immunology :专家发现器官排斥的启始分子
2017-06-24 MedSci MedSci原创
匹兹堡大学医学院和多伦多大学的研究人员发现了导致免疫系统激活和最终排斥移植器官的第一个分子步骤。今天发表在《科学免疫学》上的研究结果可能会被用于开创新方法使供体-受体能够更好的匹配,防止移植组织的排斥反应。大约50%的移植器官在10至12年内被排斥,所以非常需要更好的方法来减少或消除器官排斥反应,该研究的共同资深作者,Frank&Athena Sarris移植生物学主席和皮特的Thomas E.
匹兹堡大学医学院和多伦多大学的研究人员发现了导致免疫系统激活和最终排斥移植器官的第一个分子步骤。今天发表在《科学免疫学》上的研究结果可能会被用于开创新方法使供体-受体能够更好的匹配,防止移植组织的排斥反应。
大约50%的移植器官在10至12年内被排斥,所以非常需要更好的方法来减少或消除器官排斥反应,该研究的共同资深作者,Frank&Athena Sarris移植生物学主席和皮特的Thomas E. Starzl移植研究所(STI)的科学主任Fadi Lakkis解释道。
Lakkis 说:"我们第一次对排斥反应的初始阶段有了初步认识。" "打破固有免疫系统对外来组织的初始识别,在早期的初始阶段会干扰排斥反应,并能防止移植失败。"
在过去35年的时间里,UPMC一直是器官移植领域的全球领先者。纵观历史,匹兹堡大学移植研究所于1996年更名为STI,以纪念肝移植先驱者Thomas E. Starzl博士,该研究所一直致力于移植策略的创新性研究。
"这项研究是STI致力于改善器官衰竭患者生活质量的最新案例。"Lakkis说。
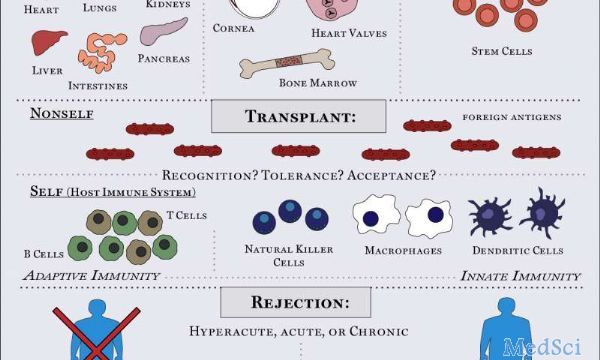
免疫系统分为固有免疫和适应性免疫。固有免疫系统首先检测体内的外来细胞,并激活适应性或获得性免疫系统。器官移植后免疫激活的第二阶段的机制已经得到了充分的研究,但是迄今为止,关于固有免疫如何导致排斥的细节还不清楚。在新研究中,研究人员使用经典的遗传作图方法来证明在小鼠中称为SIRP-α的分子导致固有免疫系统的激活,并且在不相关的个体之间是不同的。当移植组织SIRP-α与宿主组织SIRP-α不同时,移植物SIRP-α与位于受体单核细胞(一种固有免疫细胞)上称为CD47的受体结合。这种结合激发了一系列细胞活动,激活了固有免疫系统,并最终形成了适应性免疫系统。
Lakkis说,就像老鼠一样,人类也表达SIRP-α,因此对基因进行测序,以确定捐赠者和受体的匹配形式,这有望在未来降低器官排斥率。
阻断小鼠中SIRP-α和CD47之间的相互作用阻止了单核细胞的活化,这表明这种偶联的破坏作用可能会阻止受体免疫系统的激活。未来的研究,通过检查SIRP-α和CD47之间的相互作用如何导致单核细胞活化可能会引发新的方法来预防器官排斥反应。
原文出处: H. Dai el al., "Donor SIRPα polymorphism modulates the innate immune response to allogeneic grafts," Science Immunology (2017).
此文系梅斯医学(MedSci)原创整理编译,转载须授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#排斥#
25
#SCIE#
28
感谢分享!继续关注!
39
学习了受益匪浅
43
学习,谢谢分享
48
学习了。。。。
40