白细胞和血小板异常增高,血涂片镜下大量散在、不定形物质是个啥?
2021-11-29 王言 | 吉林大学第二医院检验科 吕晓艳 | 吉林大学第二医院检验科 赵凤莲 | 吉林大学第二医院检验科 卢雪红 | 吉林大学第二医院肾病内科 检验医学
一起来探案!
冷球蛋白是一种含有类风湿因子的单克隆或多克隆免疫球蛋白。近年来研究发现冷球蛋白血症与肝炎病毒感染、免疫系统疾病、恶性肿瘤疾病相关,可引起多种临床症状,其中肾脏经常受累,出现各种病理类型的肾炎[1-2],本病例即为一例慢性肾病5期的患者。
由于临床上碰到冷球蛋白血症的病例较少,检验科医生对这种特殊标本的认识不足,若不细心观察仪器相关图形、报警信息以及镜下细胞形态和特殊成分,很难为临床回报正确的检验数据,往往给临床的诊治工作带来困扰。在血常规检测中,冷球蛋白血症的标本不仅影响了血小板的计数,我们还发现对于电阻抗法检测白细胞总数也产生了很大的影响,导致了白细胞和血小板数的假性增高。
患者,男性,54岁,因“间断性四肢水肿、规律透析5年,间断性发热3个月”于2021年4月2日入我院肾病内科诊治。患者因发热入院,初步诊断为“慢性肾脏病5期、缺血性心脏病、高血压病3级”。
入院辅助检查:白细胞计数(WBC)4.8×109/L、红细胞计数(RBC)2.82×1012/L↓、血红蛋白含量(HGB)76g/L↓、血小板计数(PLT)257×109/L、总蛋白(TP)54.4g/L↓、白蛋白(ALB)34.6g/L↓、球蛋白(GLB)19.8g/L↓、尿素氮(BUN)33.04mmol/L↑、肌酐(Cr)776umol/L↑、尿酸(UA)645umol/L↑、脂蛋白(a)1147.9mg/L↑,B型钠尿肽(BNP)2445.0pg/mL↑、血清蛋白电泳:α1球蛋白6.9%↑、α2球蛋白21.2%↑、β球蛋白11.0%、γ球蛋白4.8%↓,免疫球蛋白G2.55g/L↓、补体C42.92mg/dL↓、类风湿因子(RF)1030.0IU/mL↑。
4月12日患者复查血常规,发现白细胞和血小板均异常增高。白细胞计数(WBC)40.2×109/L↑、血小板计数(PLT)645×109/L↑。
随后的一周时间内,患者的WBC和PLT计数波动较大(如图1-2)。WBC计数最高达63.6×109/L,随后还可以在正常值范围内8.7×109/L。PLT计数最高达645×109/L,或者126×109/L。究竟什么原因导致这两项指标在短期内波动这么大,我内心充满了疑问。
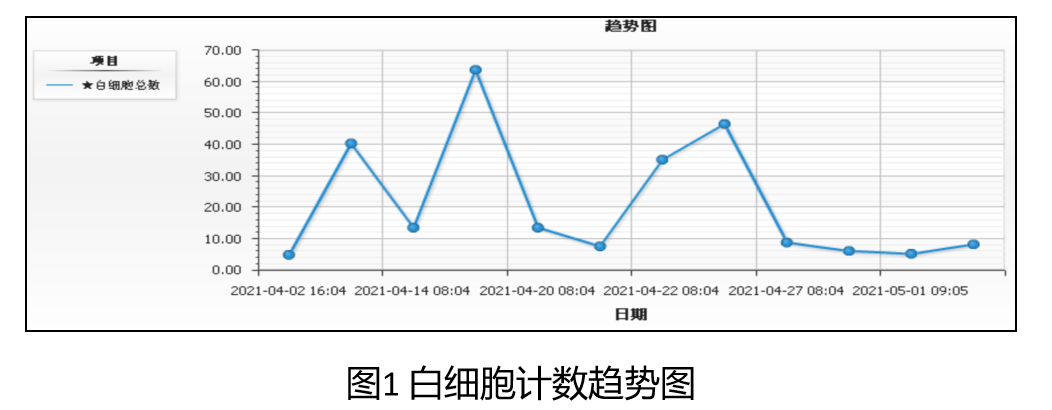
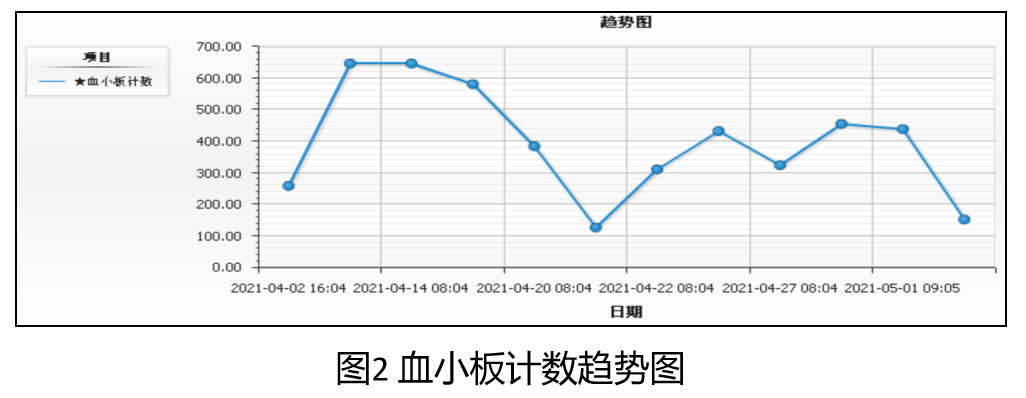
该患者WBC和PLT检测结果上下波动引起了我们的注意,通过对几次结果回顾性观察,我们发现,WBC和PLT计数值较高时,多是采用品牌1血细胞分析仪进行检测,而WBC计数正常,单纯PLT计数升高时,多是采用品牌2血细胞分析仪进行检测。
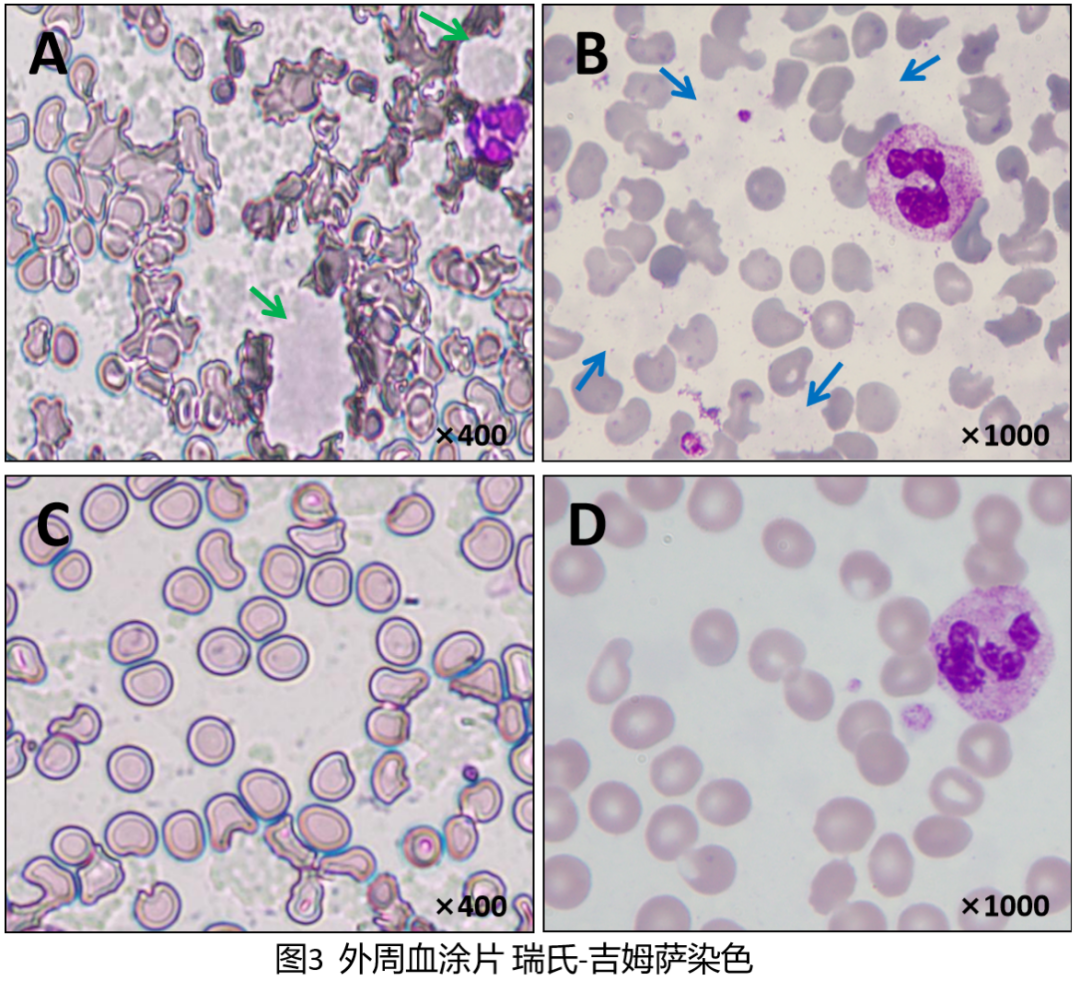
我们在和临床医生积极沟通后,希望重新采集标本进行检测。在常温和37℃温育后,分别采用两台仪器对标本进行检测,结果见(表1)。同时将检测后的标本进行涂片、染色后镜下观察。
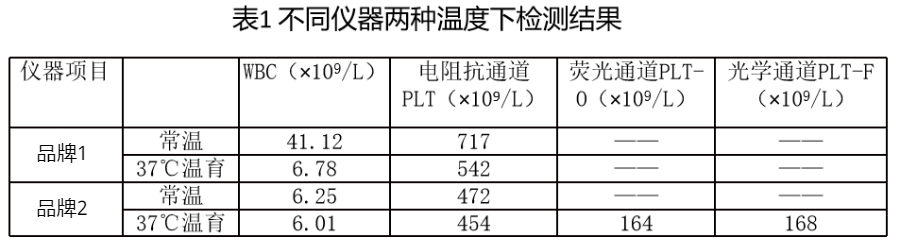
首先,常温标本血涂片高倍镜下发现大量散在、不定形物质,其染色较淡,呈灰白色颗粒状或片状,同时这些物质使得周围红细胞的形态发生了改变,呈盔形或半月形等;油镜下这些不定形物质颜色明显变淡,呈絮状模糊淡影,不易观察(如图3-A、B);
显微镜直接计数法估算PLT为151×109/L,WBC约5×109/L,明显与品牌1测得的数据PLT 717×109/L,WBC 41.12×109/L有较大的差异。
我们意识到,可能是这些片状物质干扰和影响了仪器的检测。将标本37℃温育30min后,再次进行涂片观察,片状物质明显减少,但并没有完全消失,而周边红细胞形态大致恢复正常(如图3-C、D),显微镜直接计数法再次估算PLT为160×109/L,WBC 6×109/L,此时品牌1复测数据为6.78×109/L,与显微镜下估算值接近。
注:A、B为室温标本;C、D为37℃温育后标本
↑大片状灰白色冷球蛋白沉淀 ,↑絮状淡灰白色冷球蛋白沉淀
标本经过37℃温育后可以使片状物质溶解,从而减少对检测结果的干扰。镜下的这种颗粒状或片状物质到底是什么?根据这种物质的温度依赖性以及患者慢性肾病病史和RF异常增高的特点,我们考虑是冷球蛋白血症的特殊病理性冷球蛋白。
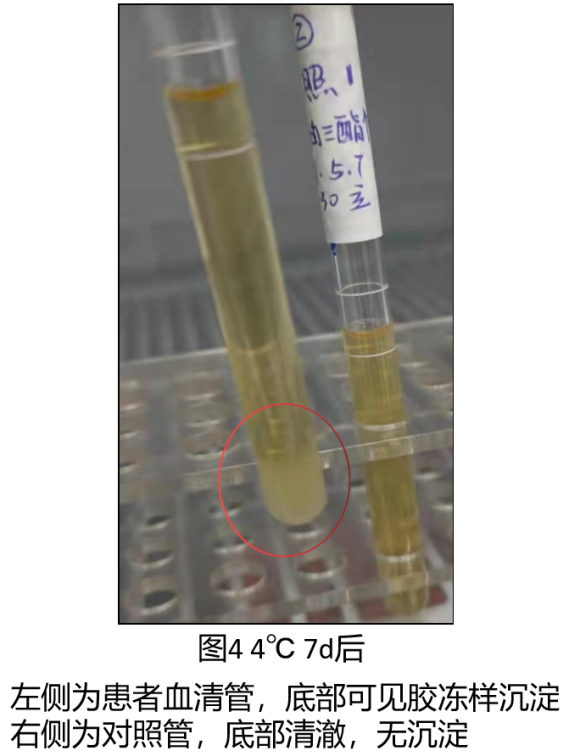
为证实猜测,我们进一步做了冷球蛋白定性试验。采集静脉血10mL到无添加剂的真空管中,37℃恒温送检,在37℃温育静置约60min后离心分离血清(在套管中加入温水),用温育后的毛细滴管吸取血清转入两只玻璃试管,分别置于37℃和4℃内7天,我们发现37℃试管中无变化,而4℃试管中形成胶冻样沉淀(如图4),之后把4℃试管放入37℃温育后,沉淀可消失,证实了我们最初的猜测,标本中有冷球蛋白的存在,冷球蛋白定性试验呈阳性反应。
值得注意的是,品牌2的荧光通道和光学通道温育前与温育后检测数据差异不大,且与我们镜检估算值基本吻合,提示冷球蛋白对该机型的检测影响较小(表1)。
该病例是一位老年男性,慢性肾脏病病史,规律透析,现因不明原因发热入院。除原发病症状外,还伴有间断腹痛、关节痛以及皮肤的改变(双手足暗褐色斑片,脚部及耳部多部位水泡及冻疮样改变)。
针对本病例,我们根据患者的临床表现及相关实验室检查,曾一度怀疑患者为成人“Still综合征”。另外,在查找发热原因的过程中,我们发现血常规结果,尤其是白细胞水平波动很大,且与临床感染程度表现不相符。
几次会诊无果后,检验科老师提示我们,患者的血常规结果受到了血清中有形成分的干扰,详细解释了冷球蛋白对于实验室部分检测结果的影响,并给出了实验室冷球蛋白定性检测的建议。综合患者的症状、体征以及检验结果,考虑冷球蛋白血症可能性大。
补充了该临床诊断后,患者之前难以解释的一些临床表现包括寒冷性肢端发绀、关节痛、寒冷性荨麻疹等表现均有了答案。但该患者引起冷球蛋白血症的原发病目前仍缺乏足够证据。我们调整了治疗方案,调节激素用量,以及改善循环、对症支持治疗,经过积极治疗后患者出院。检验科同事在该病例的诊断和鉴别诊断过程中给我们提供了重要线索和帮助,为我们临床解除了困扰。
冷球蛋白具有在低温下聚集形成沉淀,在体温37℃条件下溶解的性质。血涂片中可以表现为细胞外的不定形沉淀物,亮而薄[3]。它可直接堵塞血管并通过形成的免疫复合物激活补体系统,导致炎症反应,故常引起全身性血管炎,最常见为小动脉炎或静脉炎。血液中可检测出冷球蛋白的一类疾病被称为冷球蛋白血症[6]。
冷球蛋白可以是免疫球蛋白,也可以是免疫球蛋白与补体成分形成的复合物[4]。曾有文献报道过,冷球蛋白可以导致血小板的假性增高[5],但我们发现冷球蛋白不仅影响血小板的计数,还对不同血细胞分析仪,不同检测方法的白细胞计数产生影响。
从表1中我们可以看到在常温和37℃温育的两种状态下,品牌1检测的WBC和PLT计数值相差较大,而品牌2检测的只有PLT计数相差较大,WBC计数基本没有变化。由此可见,这种现象的发生与两种不同检测仪器息息相关。
品牌1血细胞分析仪采用电阻抗方法对白细胞和血小板数进行计数,标本中不易溶解的红细胞、聚集的血小板、巨大血小板、有核红细胞、冷球蛋白等是白细胞和血小板计数的干扰因素。
电阻抗法检测白细胞和血小板时,会将标本中不同大小的冷球蛋白沉淀颗粒错误地识别为白细胞或血小板,导致二者计数结果假性增多。通过对品牌1血细胞分析仪相关参数及图形的观察分析,我们发现,品牌1血细胞分析仪检测常温标本时存在以下异常(如图5):
1. 研究参数处WBC和UWBC检测值相差较大;
2. 三个报警信息分别是:Abn NRBC Pattern、Cellular inter、Platelet Clumps,分别提示异常NRBC群、35fl处存在干扰(可以是血小板聚集、巨大血小板、有核红细胞、冷球蛋白)、PLT聚集或凝块。
3. 白细胞直方图中可以见到一个波峰,同时这个波峰位于横坐标轴起始35fl处,这与报警信息提示相吻合;红细胞直方图未见明显变化;血小板直方图显示主峰明显左移,且左侧上升曲线较平直。
4. 白细胞散点图显示在单核细胞和中性粒细胞的交界处出现了融合散点,导致两种细胞的边界不清晰。
同时,通过对37℃温育标本检测结果分析发现,与常温标本检测结果对比(见图5),除WBC和UWBC数值明显降低、散点图处单核细胞和中性粒细胞边界稍清晰外,其报警信息、直方图处均未见明显改变(见图6)。所以,针对与37℃温育后的标本,品牌1血细胞分析仪只是纠正了WBC计数值,而PLT计数值没有得到纠正。
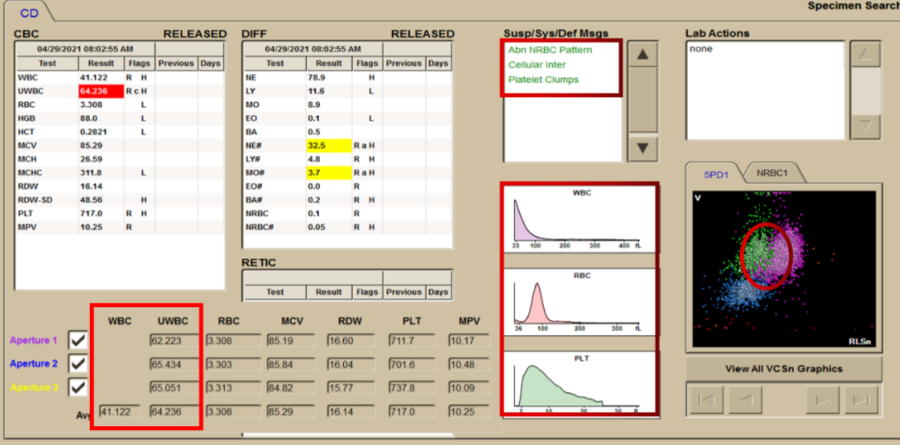
图5 常温品牌1血细胞分析仪检测结果
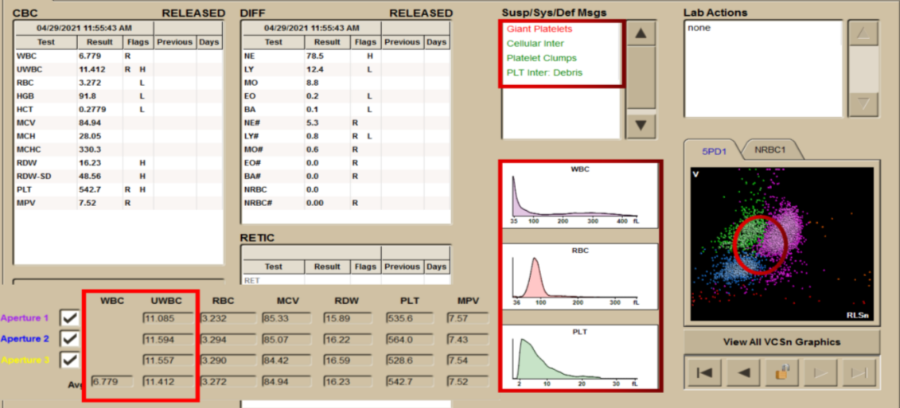
图6 37℃温育品牌1血细胞分析仪检测结果
品牌2常规检测PLT时,也采用的电阻抗方法,所以冷球蛋白也会导致PLT计数的假性增高。但品牌2血细胞分析仪的PLT-F通道中,采用了核酸荧光染色技术和41℃的恒温加热功能,用Fluorocell PLT荧光染料对血小板进行特异性染色,根据前向散射光和荧光强度的差异,品牌2血细胞分析仪的光学通道可以排除红细胞及其他干扰物质的干扰,准确检测PLT;
而品牌2血细胞分析仪的荧光通道(PLT-O),也具有41℃恒温加热的功能,可以很好地消除冷球蛋白对PLT检测的干扰。
对于WBC的计数,品牌2采用的检测方法是半导体激光的流式细胞术,分析以波长633nm激光照射细胞所得的前向散射光(FSC)、侧向散射光(SSC)、侧向荧光(SFL),将细胞进行计数。其中两种散射光(FSC、SSC)反应细胞大小、表面结构、颗粒形状、核形、折射率和反射率等。
一般情况下,细胞越大,FSC的信号就越强,细胞内部构造越复杂,SSC的信号也越强。另外,侧向荧光(SFL)主要反映细胞内核酸和细胞器的种类和多少。通过这三种信号,可以很好的对WBC进行计数分析。
本病例中,无论是在常温条件下,还是37℃温育后,对于WBC计数和PLT计数,品牌2血细胞分析仪在检测时均未见相关报警信息,WBC散点图和PLT直方图亦未见异常,故对于PLT的检测来说易造成漏诊(见图7-8)。所以,在日常标本检测时,我们应该结合报警信息、直方图和散点图综合分析,对于结果异常的标本,需要人工显微镜确认干扰,并纠正相关项目计数值。
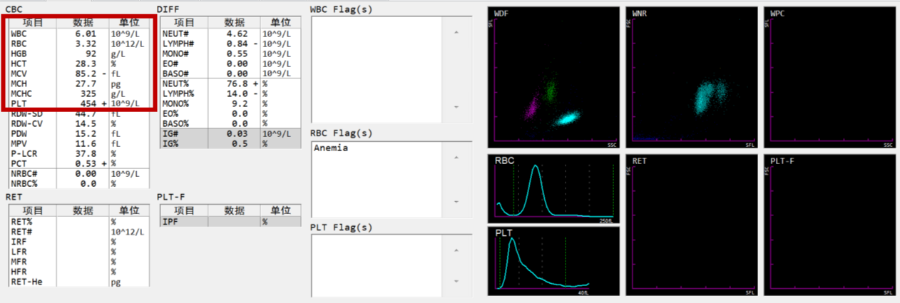
图7 常温品牌2血细胞分析仪检测结果
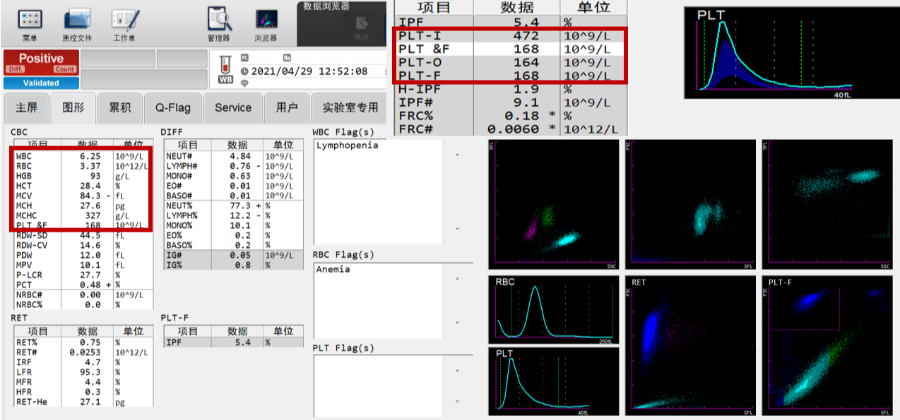
图8 37℃温育品牌2血细胞分析仪检测结果
冷球蛋白血症患者的临床表现为乏力、皮肤紫癜、关节痛、肾小球肾炎、部分患者出现肾病综合征、急性肾衰,临床上要予以一定的重视[4]。对于检验科来说,冷球蛋白对多项实验室指标的检测均有影响,容易给临床的诊治工作带来困扰,影响治疗效果。
不同血细胞分析仪的检测原理不一致,其受干扰的影响因素也不相同。如果血常规检测遇到直方图异常或有异常报警信息时,需要涂片镜检确认。对于疑似有冷球蛋白影响的标本,我们需要采取正确有效的处理方法:
1. 与临床及时沟通,在37℃恒温条件下保存和运输标本,并尽早完成检测;
2. 检测时应开启PLT-F通道或者光学通道,以确保回报准确的检测结果;
3. 在外周血涂片中发现疑似冷球蛋白物质时要积极与临床医生联系,为患者进一步诊断提供线索与帮助。
我们所从事的临床检验工作,平凡中自有不平凡,因为我们所面对的每一份标本背后,都是一个鲜活的生命,值得我们去尊重。为临床提供有效信息、回报准确的报告一直是我们检验人所履行的职责!
本案例中在没有临床相应干预的前提下,患者外周血血细胞计数在短时间内发生了很大的波动,给临床诊治工作带来了困扰,作者通过对白细胞和血小板数值进行回顾性分析后,发现数据的波动与血细胞分析仪型号相关。
在对外周血涂片中不明物质进行仔细观察后,考虑标本中存在冷球蛋白,并影响了检测结果,经过定性实验检测后证实了最初的判断,最终为临床明确冷球蛋白血症的诊断提供了重要线索。案例真实、不期而遇、认真思考、冷静对待,为临床进一步诊治提供有价值的实验室线索也是检验人员为患者负责任的具体表现!
专家简介:赵丽艳,医学博士,主任医师,副教授,硕士研究生导师,吉林大学第二医院检验科教研室主任
参考文献:
[1]袁同玲,赵毅,张伶姝,等.32例冷球蛋白血症患者临床、血清学和病理学特点[J].科学技术与工程,2020,20(23):9302-9307
[2]苗林子,屈晨雪,龚岩,等.冷球蛋白血症与肾小球肾炎:对187例患者的回顾分析[C]//第一次全国中西医结合检验医学学术会议.北京:中国中西医结合学会,2014:275-276.
[3]Fohlen-Walter A,Jacob C,Lecompte T,et al.Laboratory identification of cryoglobulinemia from automated blood cellcounts,fresh blood samples,and blood films[J].Am J Clin Pathol,2002,117(4):606-614.
[4]Canetta P A,Nestor J G.Mixed cryoglobulinemia[J].Glomerulonephritis,2019,26:459-472.
[5]于连辉,王庚等.冷球蛋白血症致血小板计数假性正常1例[J].临床检验杂志,2014,32(10):799-800.
[6]史晓虎,马杰,李 超,等.30例冷球蛋白血症病例特点分析[J].中国医学科学院学报,2014,36(6):639-644.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
52
#血涂片#
43
#增高#
51
#增高#
43
冷球蛋白
55
学习了。
49
好
50
学习了
58