本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2017-08-10 zhangfan MedSci原创
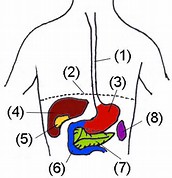
胃食管反流病的治疗指南

以往的报道还没有系统地描述过在一般人群中慢性咳嗽的危险因素。最近研究者使用哥本哈根普通人群研究的14669例个体的数据,分别在个体层面和社区层面上对慢性咳嗽危险因素进行了识别和分级。并将结果发表在医学知名期刊Chest上。
由此可见,该研究基于336例经常出现上消化道症状患者的数据分析,总上皮厚度是诊断GERD的一个很重要组织学标志。
Mederi Therapeutics 今天宣布,有关Stretta疗法的最新十年期患者随访数据已在今年的欧洲联合胃肠病学周 (United European Gastroenterology Week,简称 UEGW) 上发布。
本文是对2008年版亚太胃食管反流病共识的更新,主要聚焦在质子泵抑制剂耐药的反流性疾病和巴雷特食管。针对这些内容共提出了32条声明。全文获取:下载地址:指南下载(需要扣积分2分, 梅斯医学APP免积分下载)
胃食管反流病 (GERD) 治疗系统 Stretta 疗法生产商 Mederi Therapeutics Inc. 宣布发布病例系列,证明 Stretta 疗法可用于治疗腹腔镜缩胃手术 (LSG) 术后慢性胃食管反流病。病例系列发布在同行评议期刊《Bariatric Times》11月刊。
胃灼热是指由于食管下括约肌无法紧闭,导致食物和胃酸逆流回食道或口中所产生的灼热感觉。患者可能会出现以下表现:胸骨后及咽喉部灼热感、口味变化、咳嗽、进食后声音嘶哑等。胃灼热给患者带来的不适感可持续几个小时,严重者可出现胃食管返流疾病(GERD)。胃食管反流性疾病会导致患者频繁出现胃灼热、食物口感改变、食管损伤、失血、体重减轻。 并不是说所有的治疗治疗措施都适用于每一位患者,最安全的治疗措施应是与医生


梅斯医学MedSci APP
医路相伴,成就大医
#治疗指南#
28
#AST#
35
#胃食管#
36
#GAS#
28
#Gastroenterol#
28
学习啦!谢谢分享!
51
#反流病#
35
学习了谢谢分享
55
不错的,学习了!谢谢分享!
48
不错的指南,为我们探讨研究提供了方针,必须给点个赞了!
54