Chest:阿替普酶治疗SARS-Cov2新冠肺炎患者呼吸衰竭的研究
2021-10-15 从医路漫漫 MedSci原创
背景:肺血管微血栓是COVID19呼吸衰竭的一种可能机制。我们假设早期给予组织型纤溶酶原激活剂(tPA)并随后给予治疗性肝素可以改善这些患者的肺功能。
背景:肺血管微血栓是COVID19呼吸衰竭的一种可能机制。我们假设早期给予组织型纤溶酶原激活剂(tPA)并随后给予治疗性肝素可以改善这些患者的肺功能。
研究问题:tPA能改善严重新冠肺炎呼吸衰竭患者的肺功能吗,它安全吗?
研究设计和方法:将2020年5月14日至2021年3月3日期间患有新冠肺炎诱导的呼吸衰竭的成年人随机分为两个阶段:阶段-1(n=36):对照(护理标准)vs tPA-Bolus(50mg tPA IV-bolus,随后使用7天肝素(目标aPTT = 60-80s);第2阶段(n=14):对照vs tPA-Dillow(50mg TpA静脉推注,随后在24小时内以2mg/小时的速度滴加TpA加肝素500U/小时,然后用肝素维持APtt 60-80/7天)。如果患者在之前的4.5小时内没有进行神经病学检查或横断面脑成像,以排除中风和出血转化的可能性,则患者被排除在登记之外。主要结果是随机化后48小时PaO2/FiO2较基线有所改善。次要结果包括:48小时时PaO2/FiO2改善> 50%或PaO2/FiO2>=200(复合),无呼吸机天数(VFD)和死亡率。
结果:50名患者被随机分成两组:第1阶段:17名对照组,19tPA-滴注;第2阶段:8名对照组,6tPA-滴注。没有发生严重出血事件。在tPA-Bolus患者中,随机分组后6到168小时的PaO2/FiO2比值显著高于基线(p<0.017);对照组没有显著改善。与对照组相比,tPA-Bolus患者48小时的PaO2/FiO2比值[16.9%(-8.3-36.8)vs 29.8%(4.5-88.7),p=0.11]、综合结局(11.8%vs 47.4%,p=0.03)、室间隔缺损[0.0(0.0-9.0)vs 12.0(0.0-19.0),p=0.11]和住院死亡率(41.2%vs 21.1%,p=0.19)均无统计学意义。TPA滴注的患者没有体验到好处。
CONSORT图
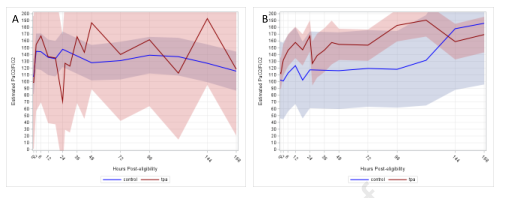
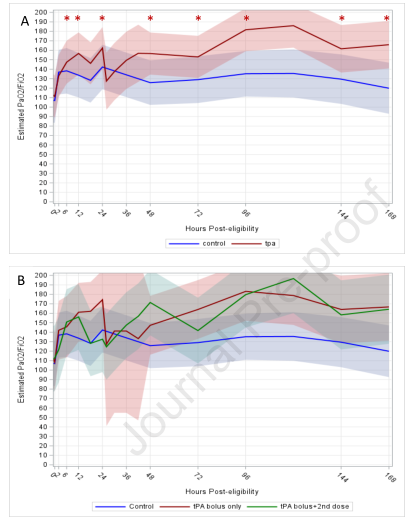
图2 A: 随着时间的推移,阶段1中的PaO2/FiO2基于tPA推注与对照组的线性混合模型(相互作用时间*干预p=0.14)以95%置信区间估计。星号表示与基线相比显着(p<0.017)差异;与基线相比,只有tPA推注组显示PaO2/FiO2显着改善;对照组PaO2/FiO2无明显改善。B:PaO2/FiO2:与A相同,但在24小时内需要第二次tPA推注,进一步分层
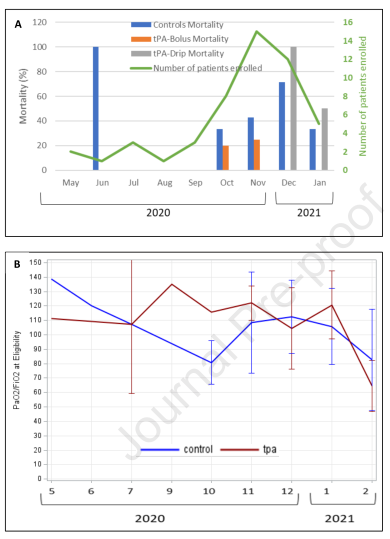
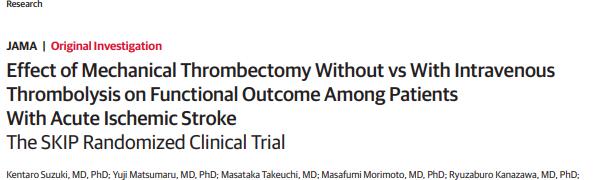
图3 试验期间疾病严重程度的趋势:A:死亡率;B:符合条件的PaO2/FiO2比率;C:符合条件的News2评分。
结论:联合应用组织型纤溶酶原激活剂+肝素治疗严重新冠肺炎呼吸衰竭是安全的。考虑到氧合作用的改善和VFD和死亡率方面的有希望的观察,3期研究是有必要的。
原文出处:
Barrett CD, Moore HB, Moore EE,et al,STudy of Alteplase for Respiratory failure in SARS-Cov2 COVID-19 (STARS): A Vanguard Multicenter, Rapidly Adaptive, Pragmatic, Randomized, Controlled Trial.Chest 2021 Sep 27
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
55
#SARS-CoV#
48
#Chest#
40
#SARS#
44