Diabetic Med:勃起功能障碍的诊断可用于改善2型糖尿病的筛查?
2018-12-25 MedSci MedSci原创
近日,国际杂志 《Diabetic Med》上在线发表一项关于勃起功能障碍的诊断可用于改善2型糖尿病的筛查的研究。评估四种未确诊的2型糖尿病风险评分对勃起功能障碍的诊断准确性。 这是一项基于人群的横断面研究。2型糖尿病根据口服葡萄糖耐量试验和自我报告的医生诊断确定。勃起功能障碍的定义是根据问题的答案,“你在过去的6个月内难以勃起吗?” (是/否)。使用的风险评分包括FINDRISC,LA-
近日,国际杂志 《Diabetic
Med》上在线发表一项关于勃起功能障碍的诊断可用于改善2型糖尿病的筛查的研究。评估四种未确诊的2型糖尿病风险评分对勃起功能障碍的诊断准确性。
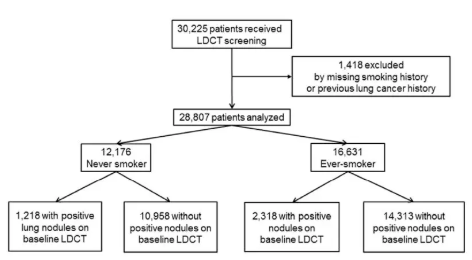
这是一项基于人群的横断面研究。2型糖尿病根据口服葡萄糖耐量试验和自我报告的医生诊断确定。勃起功能障碍的定义是根据问题的答案,“你在过去的6个月内难以勃起吗?” (是/否)。使用的风险评分包括FINDRISC,LA-FINDRISC,美国糖尿病协会评分和秘鲁风险评分。拟合泊松回归模型来评估2型糖尿病与勃起功能障碍之间的关联。接受者-操作特征曲线下的面积总体上由勃起功能障碍状态估计。
本研究共纳入799名平均(sd)年龄为48.6(10.7)岁的男性。2型糖尿病的总患病率为9.3%。与健康男性相比,患有2型糖尿病的男性患勃起功能障碍的机率为2.71(95%CI 1.57-4.66)。排除了已知2型糖尿病状态的男性(N = 38),与那些没有患有勃起功能障碍的患者相比,勃起功能障碍的三个风险评分(非美国糖尿病协会评分)的接受者-操作特征曲线下的面积得到了改善了。例如,LA-FINDRISC评分的接受者 - 操作特征曲线下面积在勃起功能障碍男性中为89.6(95%CI 78.7-99.9),总体上为76.5(95%CI 68.5-84.4)。
在一项基于人群的研究中,勃起功能障碍在2型糖尿病患者中比在其他健康男性中更为常见。在筛查2型糖尿病之前筛查勃起功能障碍似乎提高了未确诊的2型糖尿病的风险评分的准确性。
原始出处:
R. M. Carrillo,‐Larco A. C. Luza‐Dueñas,M. Urdániga‐Hung,et al. Diagnosis of erectile dysfunction can be used to improve
screening for Type 2 diabetes mellitus
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
31
#勃起#
28
#DIA#
35
#Diabetic#
33
#功能障碍#
0
#勃起功能#
27
#Med#
26
谢谢MedSci提供最新的资讯
43