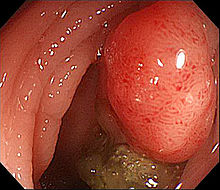
盘点:近期关于结肠癌研究进展一览
2017-11-26 lishiting MedSci原创
【1】Obes Rev:30岁以下人群肥胖也会导致结肠癌风险增加有令人信服的证据表明,成年后肥胖与结肠癌风险增加相关,但关于30岁以下人群该相关性的研究结果却是模棱两可的。近日研究人员对PubMed 和 Web of Science数据库资料进行分析,考察39岁以下人群体重指数每增加5 kg/m2与结肠癌风险的相关性。总计15项观察性研究纳入本次荟萃分析。研究发现BMI每增加5 kg/m2,会
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













讲解的非常好,值得学习
59
学习了提高了
53
#研究进展#
34
学习了.谢谢分享!
68
学习了.谢谢分享!
68
谢谢了.学习
66