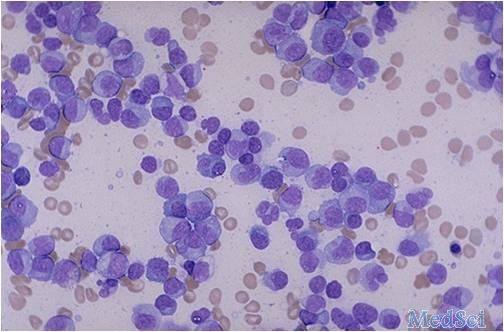
J Pathol:单胺氧化酶A(MAOA)在经典型霍奇金淋巴瘤中高表达。
2017-07-24 fengxiangxin MedSci原创
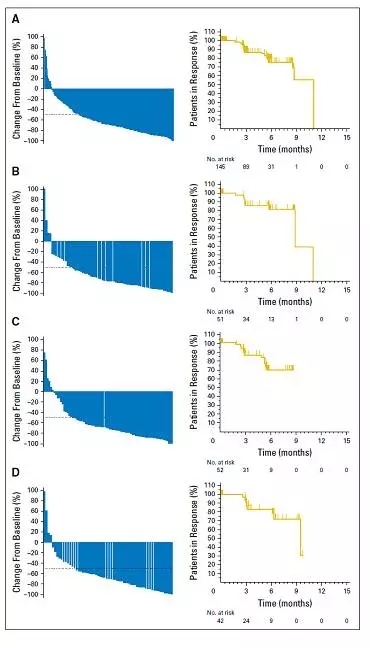
单胺氧化酶A(MAOA)是一种线粒体酶,研究表明它能够促进胶质瘤和前列腺癌的进展,但其表达和功能相关性的研究尚未在淋巴瘤中被开展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Pathol#
51
学习了.谢谢作者分享!
81
学习了受益匪浅
90
学习并分享!!!
89
精准医学时代到来的基础
112