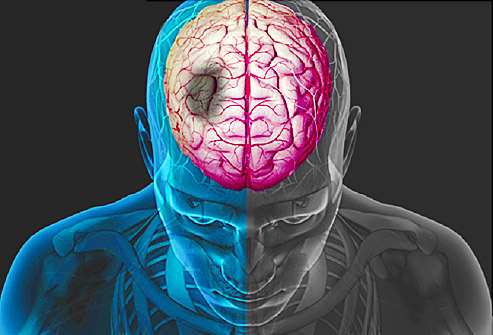
BMC Complement Altern Med:预测缺血性卒中预后的新量表
2015-11-21 MedSci MedSci原创
背景:缺血性卒中(IS)是常见疾病,常导致死亡或残疾。先前关于卒中的预后研究主要集中在基线条件或现代昂贵的检测。然而,急性状态临床症状的改变常被忽视。这篇研究旨在形成一个新的预后量表预测IS患者90天预后。方法:在这篇回顾性的队列研究中,对4个医院的1046名(排除489名)患者进行分析。新的预后预测量表主要基于3个TCM医院患者的NIHSS分数,传统中医(TCM)症状及表征,及患者前三天的变化。
背景:缺血性卒中(IS)是常见疾病,常导致死亡或残疾。先前关于卒中的预后研究主要集中在基线条件或现代昂贵的检测。然而,急性状态临床症状的改变常被忽视。这篇研究旨在形成一个新的预后量表预测IS患者90天预后。
方法:在这篇回顾性的队列研究中,对4个医院的1046名(排除489名)患者进行分析。新的预后预测量表主要基于3个TCM医院患者的NIHSS分数,传统中医(TCM)症状及表征,及患者前三天的变化。应用ROC曲线确定预测界值点。最终,这个量表在宣武医院检测IS患者的预后。
结果:这个新的预后量表包括八个条目包括年龄(OR = 3.32;95%CI:1.72-6.42),糖尿病(DM)(OR = 2.20;95%CI:1.19-4.08)NIHSS(OR = 3.08;95%CI:2.16-4.40),焦虑(OR = 3.17;95%CI:1.90-5.29),及烦躁(OR = 4.61;95%CI:1.36-15.63),卒中开始三天,NIHSS分数改变(OR= 2.49;95%CI:1.31-4.73)及旋转(OR = 7.80;95%CI:1.98-30.64)和耳鸣(OR = 13.25;95%CI:1.55-113.34)。量表的总分为16.5分,界值点为9.5,如果患者分数高于9.5分,这就意味着患者在卒中90天后预后不良。新的量表在宣武医院进行效度检验,其敏感性,特异性及整体准确率分别为69.6 %, 83.3 % 及75.0 %。
结论:主要基于TCM症状,NHISS分数及前三天的改变的8条目量表能够预测IS患者预后,但是仍需要进一步的效度检验。
原文出处:
Cao KG, Fu CH, Li HQ,et al. A new prognostic scale for the early prediction of ischemic stroke recovery mainly based on traditional Chinese medicine symptoms and NIHSS score: a retrospective cohort study. BMC Complement Altern Med. 2015,Nov 16.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMC#
26
#缺血性卒#
32
#Altern#
36
#ALT#
21
#MPL#
54
#Complement#
39
#缺血性#
21
#Med#
26