Cell Stem Cell:华人科学家找到炎症状态下影响肠癌进展的关键分子
2016-02-09 生物谷 生物谷
近日,来自美国杜克大学的研究人员发现了慢性肠道炎症与结肠癌进展之间的内在联系,这一发现不仅可以帮助找到结肠癌的早期预警信号,还可以帮助开发新的治疗方法对抗晚期结肠癌。相关研究结果发表在国际学术期刊Cell stem cell上。 肠道慢性炎症能够增加结肠癌风险,最高可达5倍。文章作者Xiling Shen这样说道:“全世界有四分之一人口受到各种肠道炎症的影响,肠炎病人发生结肠癌的风险更高,但

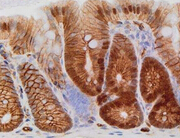
近日,来自美国杜克大学的研究人员发现了慢性肠道炎症与结肠癌进展之间的内在联系,这一发现不仅可以帮助找到结肠癌的早期预警信号,还可以帮助开发新的治疗方法对抗晚期结肠癌。相关研究结果发表在国际学术期刊Cell stem cell上。
肠道慢性炎症能够增加结肠癌风险,最高可达5倍。文章作者Xiling Shen这样说道:“全世界有四分之一人口受到各种肠道炎症的影响,肠炎病人发生结肠癌的风险更高,但是其中的原因一直没有得到很好的解释。我们在这项研究中找到了一些线索。”研究人员在这项研究中发现了一种调节细胞分裂的microRNA可能与结肠癌发展存在内在联系。
在这项研究中,研究人员主要对一种叫做miR-34a的microRNA进行了研究,这种microRNA分子与癌症干细胞不对称分裂的能力有关,能够帮助癌症干细胞维持自身群体同时产生不同类型的癌细胞。
虽然研究人员知道miR-34a具有这种能力,但是没人知道这种microRNA分子来自于哪里,正常健康的结肠干细胞并不会发生不对称分裂也不需要这种microRNA。因此研究人员对于癌症干细胞中是否存在调节该microRNA分子表达的特定突变以及这种分子在正常生理情况下是否还有其他功能这两个问题比较关注。
研究人员首先构建了miR-34a敲除小鼠,但是没有观察到明显表型。随着研究进行,问题逐渐显现:在炎症情况下如果没有miR-34a的存在,组织内的干细胞能够快速生长并失去控制,形成许多类似肿瘤的结构。
基于上述发现,研究人员认为即使miR-34a在癌细胞内发生激活,它仍然扮演着好的角色。当肠道发生炎症,miR-34a能够促进不对称分裂过程,帮助控制正常的干细胞群体。
在肿瘤生长早期,这种microRNA分子保持活跃能够抑制癌症干细胞群体,随着癌症不断进展,癌细胞产生一些基因突变能够关闭miR-34a的表达,引起细胞分裂形成一些灵活多变的混合细胞类型,这些细胞在特定情况下会重新变成干细胞,正是由于这种灵活多变的特性才使得晚期癌症变得难以治疗。
Shen表示:“一般情况下我们在肿瘤组织中发现一些健康组织中没有的分子,我们常常会认为那些是一些不好的分子。但通过这项研究我们可以看到,在正常生理环境下这些microRNA只有在机体出现问题时才会出现,如果在晚期癌症中将其沉默会导致癌症进一步恶化。”
原始出处:
Bu P, Wang L, Chen KY, Srinivasan T, Murthy PK, Tung KL, Varanko AK, Chen HJ, Ai Y, King S, Lipkin SM, Shen X.A miR-34a-Numb Feedforward Loop Triggered by Inflammation Regulates Asymmetric Stem Cell Division in Intestine and Colon Cancer. Cell Stem Cell. 2016 Feb 4;18(2):189-202.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
28
#CEL#
37
#stem cell#
34
#炎症状态#
48
太棒了!!
132
很好,值得学习
130
#STEM#
34
#华人#
34
牛
57