Nat Med:晚期肿瘤基因组突变特征研究
2017-05-09 zhangfan MedSci原创
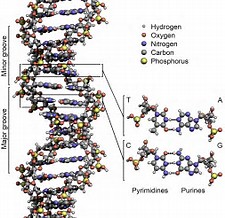
肿瘤分子分析是精密肿瘤学的基本组成部分,能够识别肿瘤细胞基因组改变实现靶向治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#晚期肿瘤#
40
#Nat#
31
继续学习中谢谢
69
学习了
66
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦……
49
#肿瘤基因#
34
#Med#
38
不错的内容,了解一下
48
内容
51
签到学习了很多。
26