Cardiovasc Res:Kcnk3 功能障碍促进左心疾病相关肺动脉高压进展
2021-10-08 刘少飞 MedSci原创
众所周知,肺动脉高压 (PH) 是左心疾病 (LHD,第 2 组 PH) 的常见并发症,可导致右心室 (RV) 衰竭和死亡。在肺动脉高压(PAH,第 1 组 PH)中发现了 KCNK3 中的几个功能丧

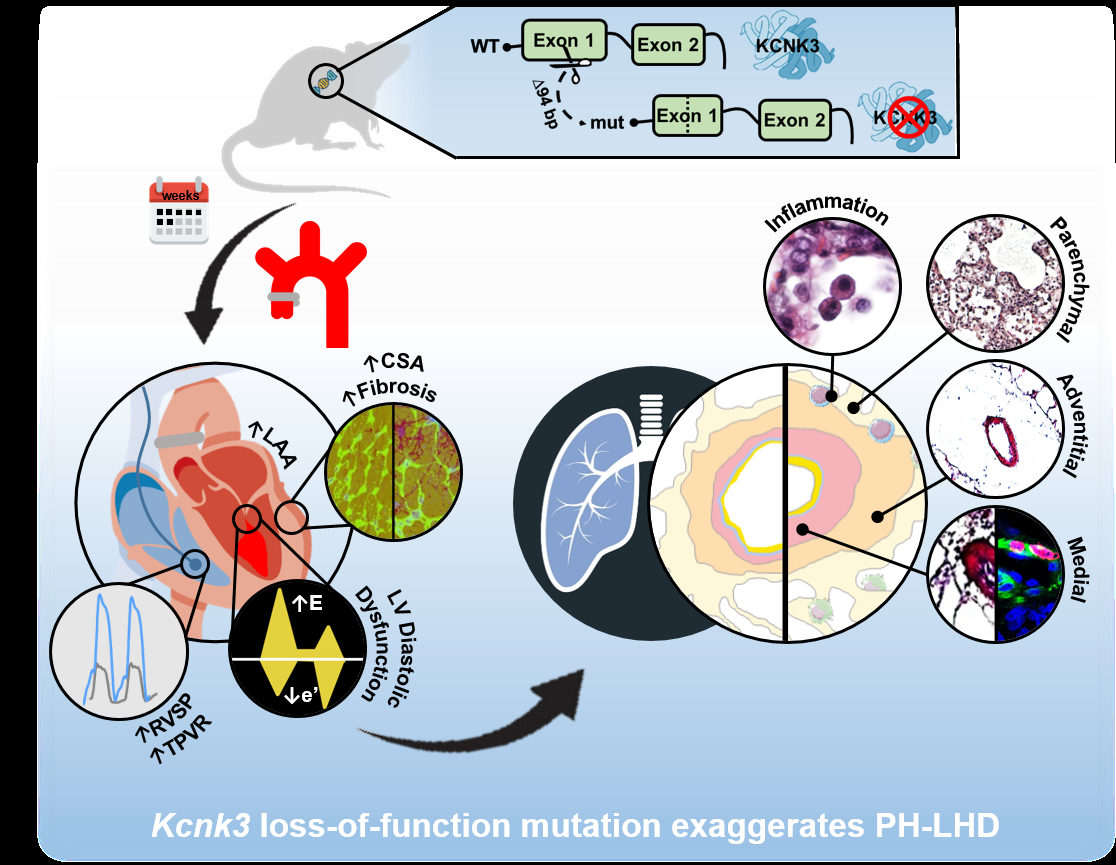
众所周知,肺动脉高压 (PH) 是左心疾病 (LHD,第 2 组 PH) 的常见并发症,可导致右心室 (RV) 衰竭和死亡。在肺动脉高压(PAH,第 1 组 PH)中发现了 KCNK3 中的几个功能丧失(LOF)突变。此外,研究发现 KCNK3 功能障碍是肺血管和 RV 水平 PAH 的标志。然而,KCNK3 在 LHD 所致 PH 病理生物学中的作用尚不清楚。
研究方法:
该研究通过超声心动图、RV 导管插入术、组织学分析和分子生物学实验评估了 KCNK3 对 WT 和 Kcnk3-LOF 突变大鼠升主动脉缩窄 (AAC) 诱导的 PH 的作用。
研究结果:
发现 Kcnk3-LOF 突变对 AAC 中左心室 (LV) 代偿性向心肥厚的发展没有影响,而 AAC-Kcnk3 突变大鼠的左心房排空分数受损。 AAC 动物(WT 和 Kcnk3 突变的大鼠)继发于 AAC,并且 Kcnk3 突变的大鼠出现了比 WT 更严重的 PH。 AAC-Kcnk3 突变的大鼠发生 RV 和 LV 纤维化,与右心室和左心室中 Col1a1 mRNA 的增加相关。与AAC-WT相比,AAC-Kcnk3突变的大鼠发生严重的肺血管(肺动脉和肺静脉)重塑,伴有强烈的血管周围和支气管周围炎症、血管周围水肿、肺泡壁增厚和肺血管细胞增殖过度老鼠。最后,在 AAC-Kcnk3 突变大鼠的肺、右心室、左心室和左心房中,发现 Il-6 和骨膜蛋白表达强烈增加,肺 Ctnnd1 mRNA(编码 p120 连环蛋白)减少,有助于AAC-Kcnk3 突变大鼠的肺和心脏重构以及肺血管水肿的夸张。
研究启示
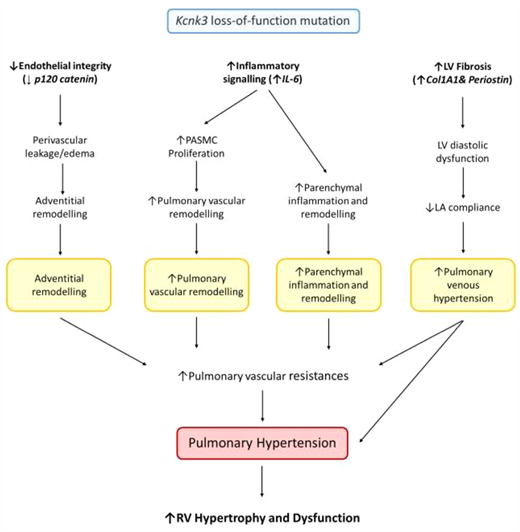
对于PAH突变KCNK3基因,其Kcnk3-LOF 是 AAC 导致的 PH 病理生物学中的关键事件,表明 Kcnk3 通道功能障碍可能在 LHD 导致的 PH 发展中发挥潜在的关键作用。在 LV 压力超负荷的背景下,该研究发现 Kcnk3-LOF 突变促进
(i) 肺内皮完整性的破坏,导致肺血管周围水肿和 PA 外膜重塑,
(ii) 炎症信号 (IL-6),导致 PASMC 增加 增殖促进肺血管和实质重塑。 (i) 和 (ii) 有助于增加肺血管阻力。
(iii) 心脏纤维化将 LV 舒张功能障碍与 LA 顺应性降低和肺静脉重构异常联系起来。
总之,这些事件有利于 Kcnk3 突变大鼠的 PH 加重和随之而来的 RV 肥大和功能障碍。
文章出处:
Lambert M. Kcnk3 Dysfunction Exaggerates The Development Of Pulmonary Hypertension Induced By Left Ventricular Pressure Overload. Cardiovasc Res. 2021 Jan 23:cvab016. DOI: 10.1093/cvr/cvab016. Epub ahead of print. PMID: 33483721.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
41
#动脉高压#
44
#功能障碍#
54
不错学习了
0