Eur Heart J:端粒长度对急性心肌梗死预后的预测价值!
2017-04-25 xing.T MedSci原创
BTL可以预测AMI后心血管事件,独立于年龄,而VTL是一种组织特异性(而不是整体)的血管氧化应激标志物。BTL和VTL之间缺乏强大的相关性表明全身和血管因素在确定AMI后临床结局的重要性。
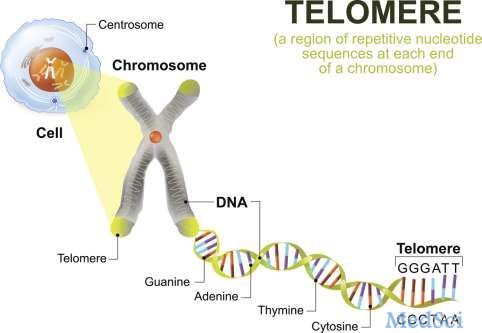
实验证据表明端粒长度(TL)可以被氧化DNA损伤所缩短,反映了生物老化。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在探讨血液中(BTL)和血管中TL(VTL)作为全身/血管在人体氧化应激指标的价值,并验证BTL在急性心肌梗死(AMI)中的临床预测价值。
在290例最近急性心肌梗死存活患者组成的前瞻性队列中,入院时测得的BTL是全因死亡[风险比(HR)[95%可信区间(CI)]:3.21[1.46-7.06],P=0.004]和心血管死亡(HR 95% [CI]:3.96[1.65-9.53],P=0.002)的主要预测因子,在AMI后1年(将短期 vs. 长期BTL进行比较,其定义为T/S比值临界值为0.916,通过ROC分析进行计算,以及调整了年龄和其他因素的P值)。
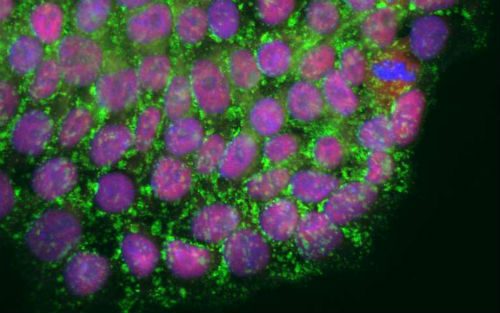
为了探讨这些结果的生物学意义,研究人员将连续就诊的727例进行冠状动脉旁路移植术(CABG)患者量化BTL,并且测量外周血单个核细胞(MNC)中的超氧阴离子(O2-)。研究人员测量了大隐静脉(SV)和乳内动脉(IMA)节段的VTL/血管O2-。患者对p22phoX(激活NADPH氧化酶)功能基因多态性进行基因型分型,并且通过基因型选择的血管平滑肌细胞(VSMC)是从血管组织中培养。在外周血单个核细胞中短的BTL与高O2-有关(P=0.04),在血管则无关,而在IMA(ρ=-0.49,P=0.004)和SV(ρ=-0.52,P=0.01)中VTL与O2-相关。采用血管紧张素II(Ang II)孵育VSMC(30天),作为刺激NADPH氧化酶,可以使高反应性p22phoX等位基因携带者增加O2-和缩短TL(P=0.007)。
BTL可以预测AMI后心血管事件,独立于年龄,而VTL是一种组织特异性(而不是整体)的血管氧化应激标志物。BTL和VTL之间缺乏强大的相关性表明全身和血管因素在确定AMI后临床结局的重要性。
原始出处:
Marios Margaritis,et al. Predictive value of telomere length on outcome following acute myocardial infarction: evidence for contrasting effects of vascular vs. blood oxidative stress. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx177
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#端粒长度#
33
#ART#
0
#HEART#
37
#预测价值#
40
多看多学!!!!
47
不错
54
不错
53