Diabetes Care:糖尿病强化和常规治疗不影响绝经时间
2014-01-13 佚名 丁香园
自然绝经和手术绝经累积发生率 为了研究糖尿病强化与常规治疗对1型糖尿病妇女绝经的影响。来自密歇根大学医学和妇产科部门的Kim博士等进行了一项研究,发现强化与常规治疗与绝经风险没有关系,而加大胰岛素剂量可降低绝经风险。研究结果在线发表于2013年12月30日的《糖尿病治疗》(Diabetes Care)杂志上。【原文出处】 研究对象来自糖尿病控制和并发症试验(DCCT)及其长期随访观察性
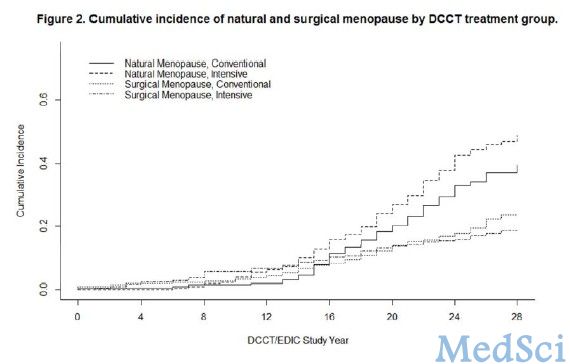
自然绝经和手术绝经累积发生率
为了研究糖尿病强化与常规治疗对1型糖尿病妇女绝经的影响。来自密歇根大学医学和妇产科部门的Kim博士等进行了一项研究,发现强化与常规治疗与绝经风险没有关系,而加大胰岛素剂量可降低绝经风险。研究结果在线发表于2013年12月30日的《糖尿病治疗》(Diabetes Care)杂志上。【原文出处】
研究对象来自糖尿病控制和并发症试验(DCCT)及其长期随访观察性研究——糖尿病干预和并发症(EDIC)研究。DCCT是一项对糖尿病强化治疗进行评价的随机对照试验。
本项研究对DCCT/EDIC试验的657名妇女的数据进行二次分析,研究结局为自然绝经和手术绝经的累积发生率。Cox线性回归分析用于评价治疗组、随时间变化的血红蛋白A1c (HbA1c)估计值、胰岛素剂量、体重指数(BMI)和微血管并发症(视网膜病变、肾病和神经病变)的相关性。
结果显示,截至EDIC研究第18年,即平均随访期28年后,自然绝经妇女为240名(38%),手术绝经妇女为115名(18%)。糖尿病强化治疗与常规治疗组妇女自然绝经年龄相似(49.9比49.0岁),手术绝经年龄也相似(40.8比42.0岁)。在多变量模型中,治疗组、HbA1c和微血管病变与自然绝经和手术绝经风险没有相关性。胰岛素剂量每增加10U/天,自然绝经风险降低(HR 0.91),而BMI每增加1 kg/m2,手术绝经风险增加(HR 1.08)。
研究表明,在DCCT/EDIC研究中,强化与常规治疗和HbA1c水平与绝经风险没有关系。加大胰岛素剂量与绝经风险降低有关。
研究背景:
两项大型的队列研究表明,1型糖尿病与较早的绝经年龄有关。在一项研究报道中,1型糖尿病妇女、她们的身体健康的姐妹和无血源关系的对照者的绝经年龄分别为41.6岁、49.9岁和48.0岁。在另一项研究报道中,1型糖尿病妇女与对照者平均绝经年龄分别为44和50岁。
多种机制有可能能够解释糖尿病对绝经时间的影响。其中一种是1型糖尿病妇女自身免疫性卵巢炎风险增加,特别是那些血循环中有肾上腺抗体的妇女。但是,肾上腺疾病对1型糖尿病妇女的影响不足5%,而其中不到1%的1型糖尿病和无临床肾上腺机能减退的妇女有肾上腺抗体存在,这样的话,用卵巢炎解释1型糖尿病妇女较早的绝经年龄不太可能。
此外,高血糖引起的卵巢组织中晚期糖化终产物蓄积可能对卵巢具有一定的毒性。糖尿病并发症(包括增值性视网膜病和肾病)的出现可能反应了卵巢微血管损伤。同时,胰岛素疗法增加每一月经周期卵泡募集,最终减少滤泡堆积,导致绝经年龄提前。
原文出处:
Kim C, Cleary PA, Cowie C, Braffett BH, Dunn RL, Larkin ME, Gatcomb P, Wessells H, Nathan DM, Sarma AV; for the DCCT/EDIC Research Group.Effect of Glycemic Treatment and Microvascular Complications on Menopause in Women with Type 1 Diabetes in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Cohort.Diabetes Care. 2013 Dec 30. 【原文出处】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#DIA#
43
#Diabetes#
37
#BET#
44
#常规治疗#
38
#绝经#
28