Nat Immunol:又犯傻了!中国科学家发现巨噬细胞竟会接受癌细胞“贿赂”,令先天免疫对病毒“网开一面”
2018-01-23 代丝雨 奇点网
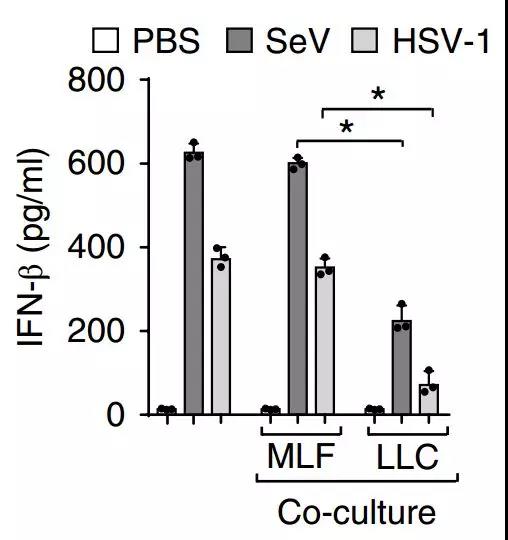
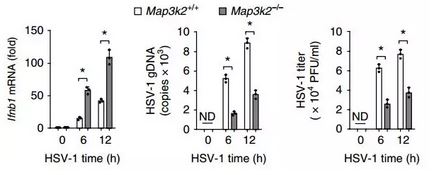
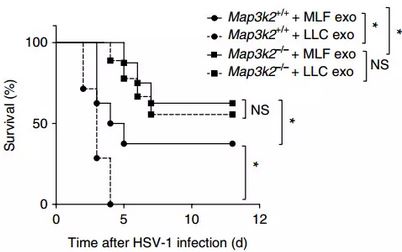
本周的《自然免疫学》上,来自浙江大学张龙课题组与苏州大学周芳芳课题组,为我们带来了一项开拓性的研究。研究者们首次发现,癌细胞会通过外泌体给巨噬细胞“送礼”,受贿的巨噬细胞被资本腐蚀,内部产生一系列变化,导致先天性抗病毒免疫功能被抑制,这或许可以解释为什么癌症患者常常免疫力低下,易染上其他疾病。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#中国科学#
28
#Nat#
40
学习了谢谢
64
#科学家发现#
29
提供了很好的病例
62
好
65
很好的文章.学习了
51
学习.
47
#癌细胞#
33
#中国科学家#
30